Immediate Implant Placement: The 2025 Evidence-Based Guide for Clinical Success

Table of Contents
The decision of when to place a dental implant after tooth extraction remains one of the most consequential choices in implant dentistry. Get it right, and you achieve predictable osseointegration with optimal esthetics. Get it wrong, and you face complications that could have been avoided with better timing.
After three decades in implant dentistry, I've witnessed the evolution from dogmatic waiting periods to evidence-based decision-making. The 2024-2025 research has finally given us clarity on what works, what doesn't, and—most importantly—why.
This guide synthesizes the latest systematic reviews and meta-analyses to help you make informed decisions about implant placement timing.
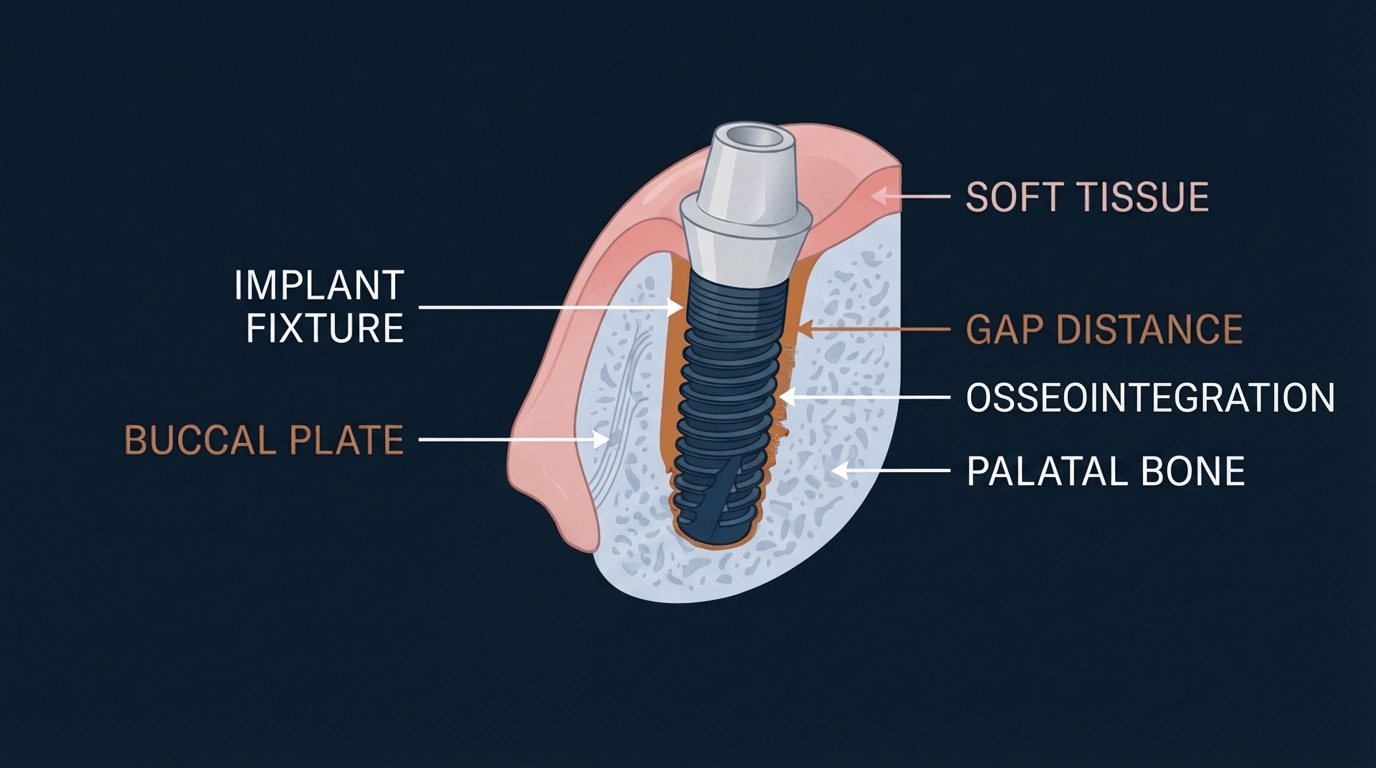
Cross-sectional view of immediate implant placement showing palatal positioning within the extraction socket (Created with periospot-studio.com)
Understanding Implant Placement Timing: The Classification System
The ITI consensus and subsequent modifications by Chen and Buser established four distinct categories of implant placement timing, each with specific biological and clinical implications:
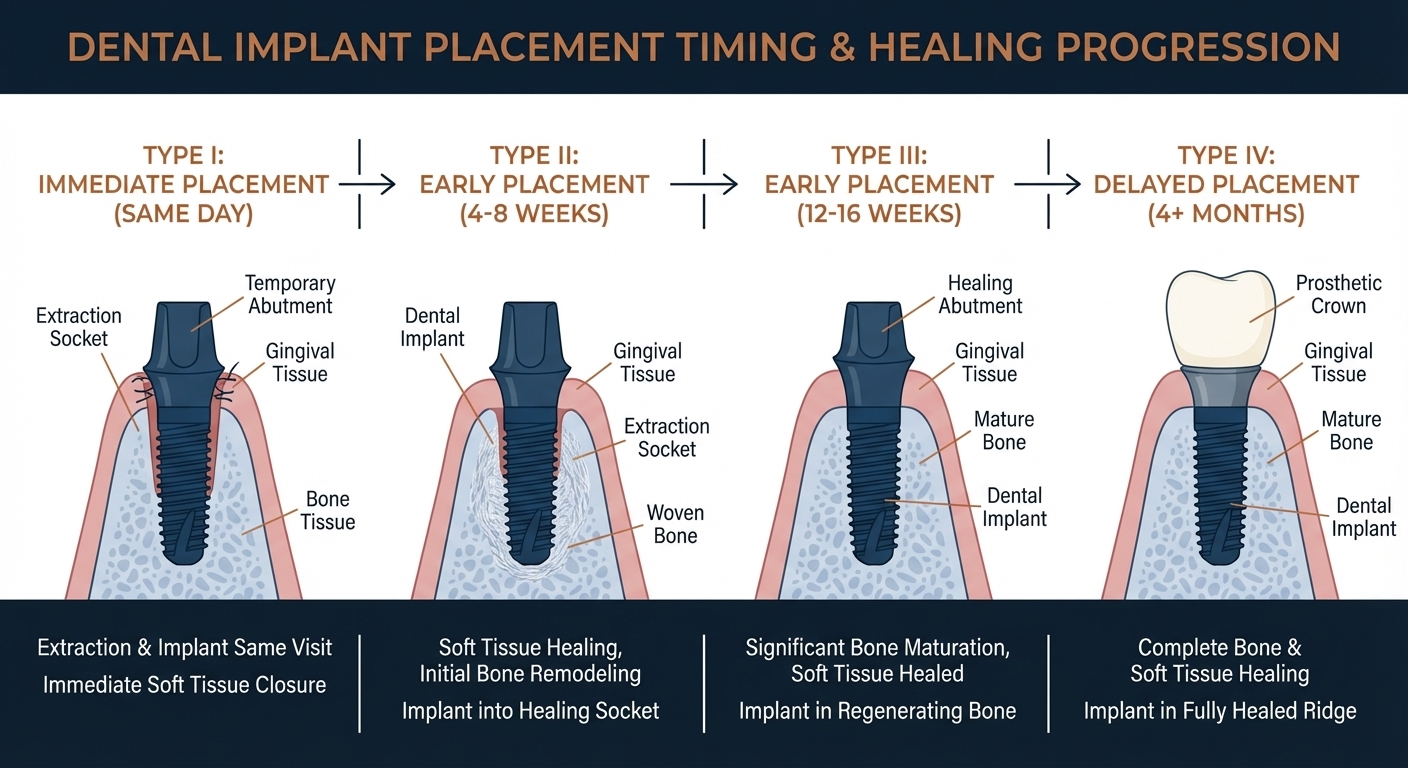
The four types of implant placement timing from immediate to delayed (Created with periospot-studio.com)
Type I — Immediate Placement
Implant placed directly into the extraction socket on the same day. This approach requires ideal conditions: intact buccal bone, thick biotype, and the ability to achieve primary stability.
Type II — Early Placement with Soft Tissue Healing (4-8 weeks)
Allows complete soft tissue coverage while bone remodeling is still active. Inflammation has resolved, but significant dimensional changes are ongoing.
Type III — Early Placement with Partial Bone Healing (12-16 weeks)
Substantial bone fill has occurred within the socket. This timing is particularly favorable for multi-rooted tooth sites.
Type IV — Delayed Placement (4+ months)
Complete bone and soft tissue healing. Most predictable but requires the longest treatment timeline.
The Biology of Socket Healing: Why Timing Matters
Understanding the biological cascade following tooth extraction is fundamental to making informed timing decisions.
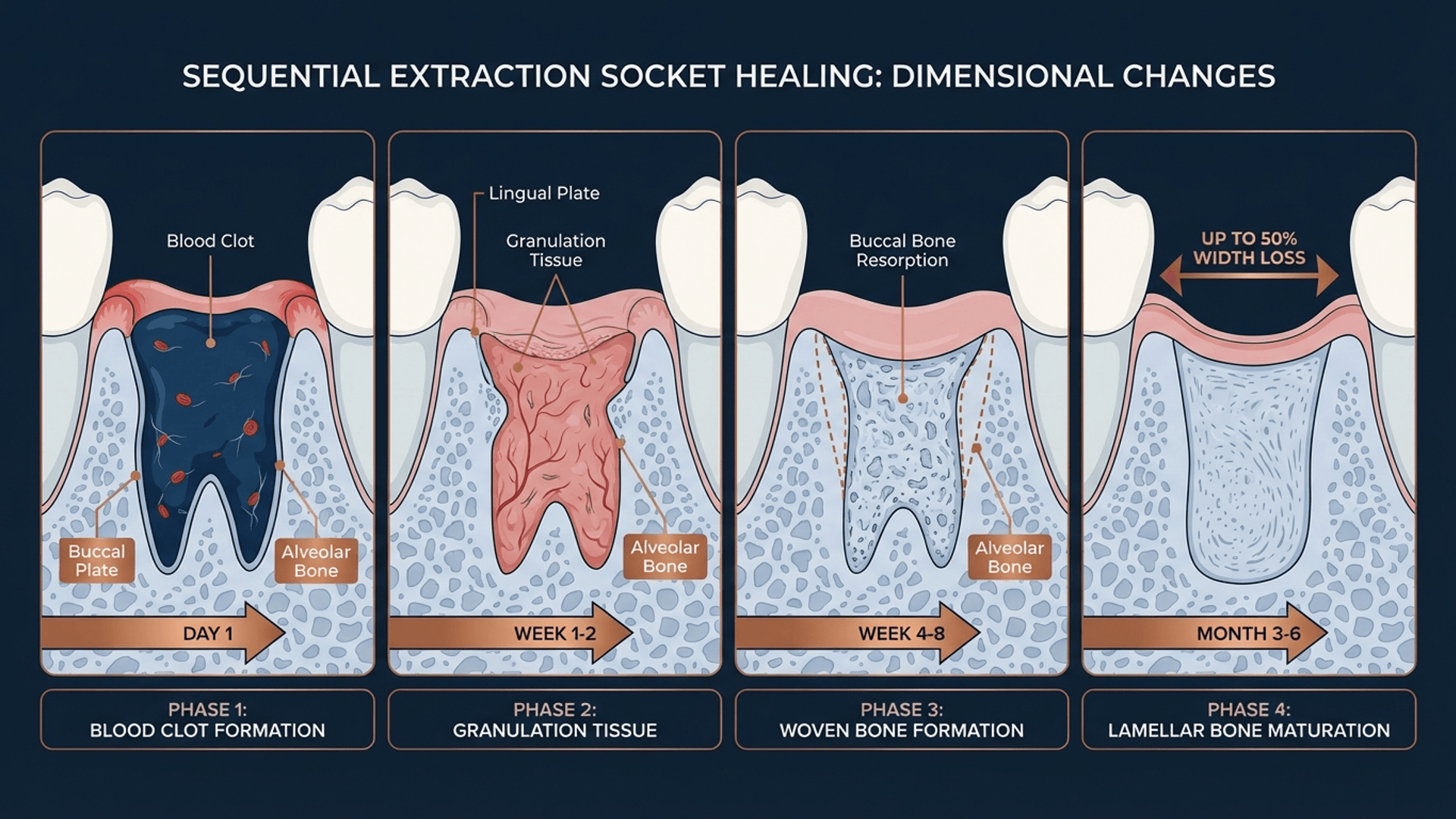
The four phases of extraction socket healing and dimensional changes (Created with periospot-studio.com)
The alveolar ridge undergoes dramatic dimensional changes post-extraction:
- Width reduction: Up to 50% within the first year, primarily in the first 3 months
- Height reduction: 2-4mm on average, more pronounced on the buccal aspect
- Bundle bone resorption: This tooth-dependent bone begins resorbing immediately after extraction
A 2024 systematic review by Chappuis and colleagues confirmed that the buccal bone wall—particularly the coronal third—is most susceptible to resorption. This has direct implications for implant placement in the esthetic zone.
What the 2024-2025 Research Tells Us
Survival Rates Across Timing Protocols
A February 2025 narrative review in the Journal of Clinical Medicine analyzed 9,774 articles and found remarkably consistent survival rates across all timing protocols:
| Placement Type | Survival Rate | Key Considerations |
|---|---|---|
| Immediate (Type I) | 93.8–100% | Technique sensitive, requires ideal conditions |
| Early (Type II/III) | 95–100% | Fewer complications than immediate |
| Delayed (Type IV) | 92–100% | Most predictable, longest timeline |
The critical insight: survival rates are comparable, but complication profiles differ significantly.
Immediate vs. Delayed: The Meta-Analysis Evidence
A groundbreaking meta-analysis published in January 2025 comparing immediate versus delayed placement in periodontitis patients found:
- Pink Esthetic Score (PES): Immediate placement showed superior outcomes
- Marginal bone loss: Comparable between groups
- Probing depth: Slightly higher in immediate placement (mean difference 0.32mm)
- Modified plaque index: Immediate placement demonstrated better scores
Another 2025 network meta-analysis comparing placement and loading protocols for anterior maxillary implants concluded that immediate implantation with immediate loading showed considerable esthetic advantage over later rehabilitation protocols, with clinically relevant improvements in pink esthetic scores.
The Periodontitis Question
For patients with a history of periodontitis—a common clinical scenario—the evidence supports that immediate implant placement can be successful with proper patient selection and meticulous surgical technique. However, residual alveolar bone height of at least 4mm post-extraction is essential for predictable outcomes.
Success Factors for Immediate Implant Placement
Not every extraction site is suitable for immediate implant placement. The research consistently identifies these critical success factors:
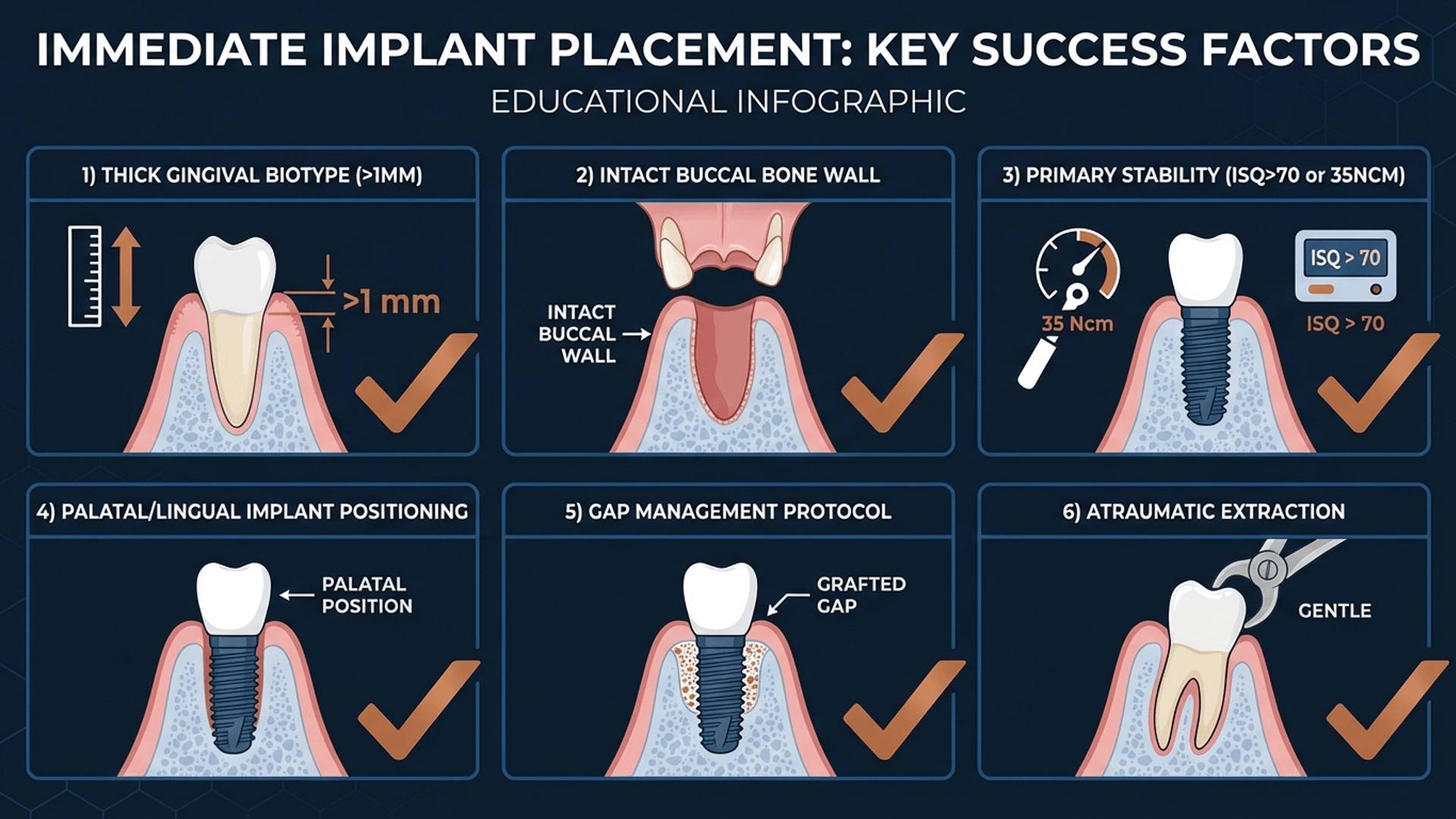
Key prerequisites for successful immediate implant placement (Created with periospot-studio.com)
1. Intact Buccal Bone Wall
The facial bone wall must exceed 1mm in thickness. A 2025 systematic review on immediate implant placement in intact versus non-intact sockets demonstrated that buccal bone thickness is the primary determinant of long-term esthetic outcomes.
2. Thick Gingival Biotype
Patients with thin gingival phenotype have significantly higher risk of recession and esthetic complications. The thick biotype provides a buffer against the dimensional changes that occur during healing.
3. Primary Stability
Achieving adequate primary stability is non-negotiable:
- Insertion torque: Minimum 25-35 Ncm
- ISQ value: 70 or greater
- Implant positioning: At least 3mm apical to the alveolar crest
4. Palatal/Lingual Positioning
The implant must be positioned palatally or lingually within the socket to minimize exposure risk as the buccal bone undergoes resorption. This creates a gap between the implant and buccal wall that requires management.
5. Atraumatic Extraction
Preserving socket integrity begins with the extraction technique. Periotomes, luxators, and vertical sectioning for multi-rooted teeth minimize trauma to the surrounding bone and soft tissue.
Gap Management: The Critical Variable
The gap between the implant surface and the buccal socket wall is perhaps the most important variable in immediate implant success.
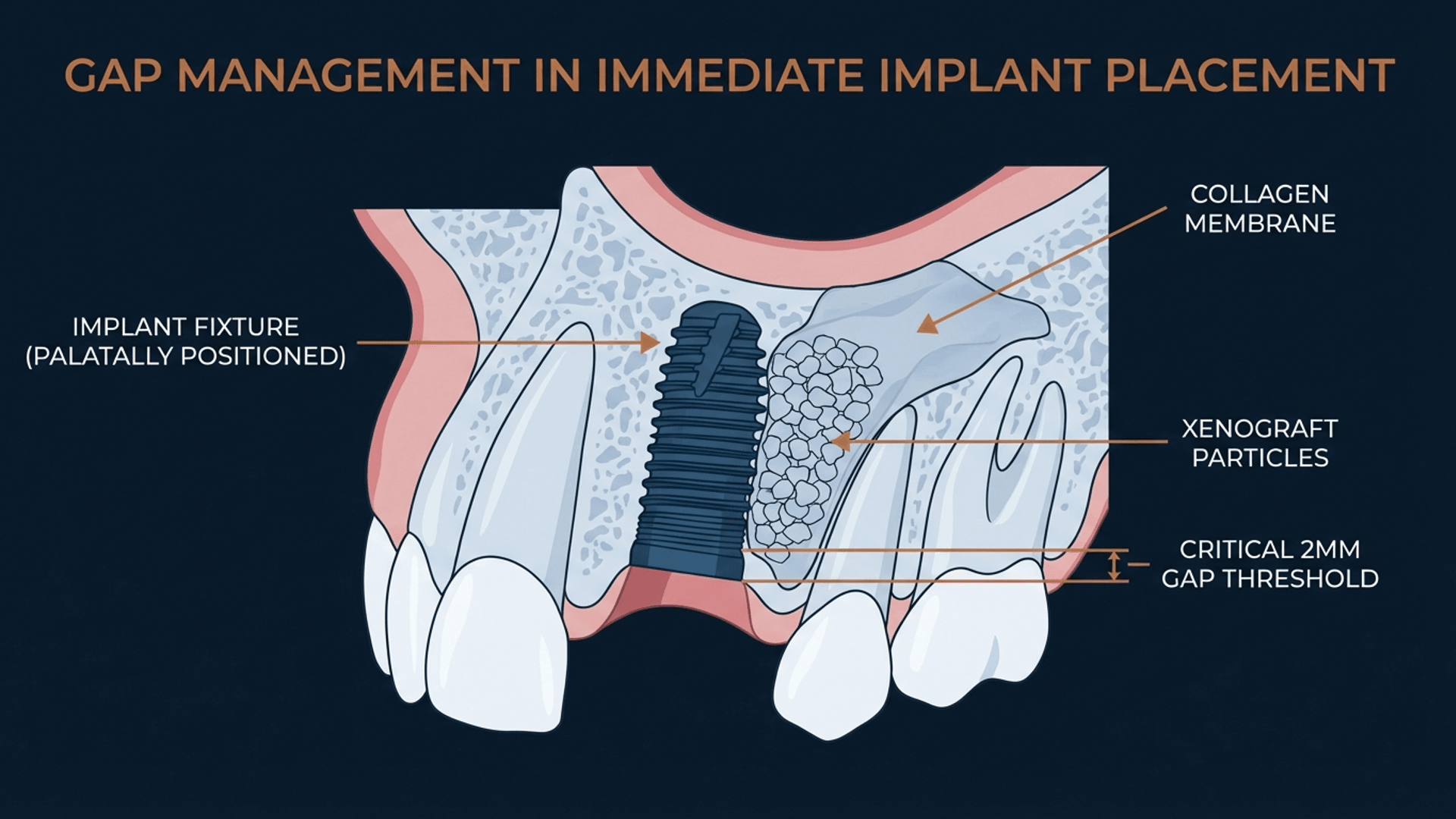
Bone grafting technique for managing the buccal gap in immediate implants (Created with periospot-studio.com)
The 2mm Threshold
Research indicates that gaps smaller than 2mm may heal spontaneously through blood clot organization. However, gaps larger than 2mm benefit significantly from grafting with a slowly resorbing xenograft material.
Grafting Protocol
The 2024 systematic review on tissue grafts with immediate implants found that both hard and soft tissue grafting improve outcomes:
- Bone grafts: Reduce dimensional changes and improve implant stability
- Connective tissue grafts: Increase soft tissue thickness and reduce recession risk
- Combination approach: May offer optimal results in esthetic zone cases
Clinical Decision-Making: When to Use Each Protocol
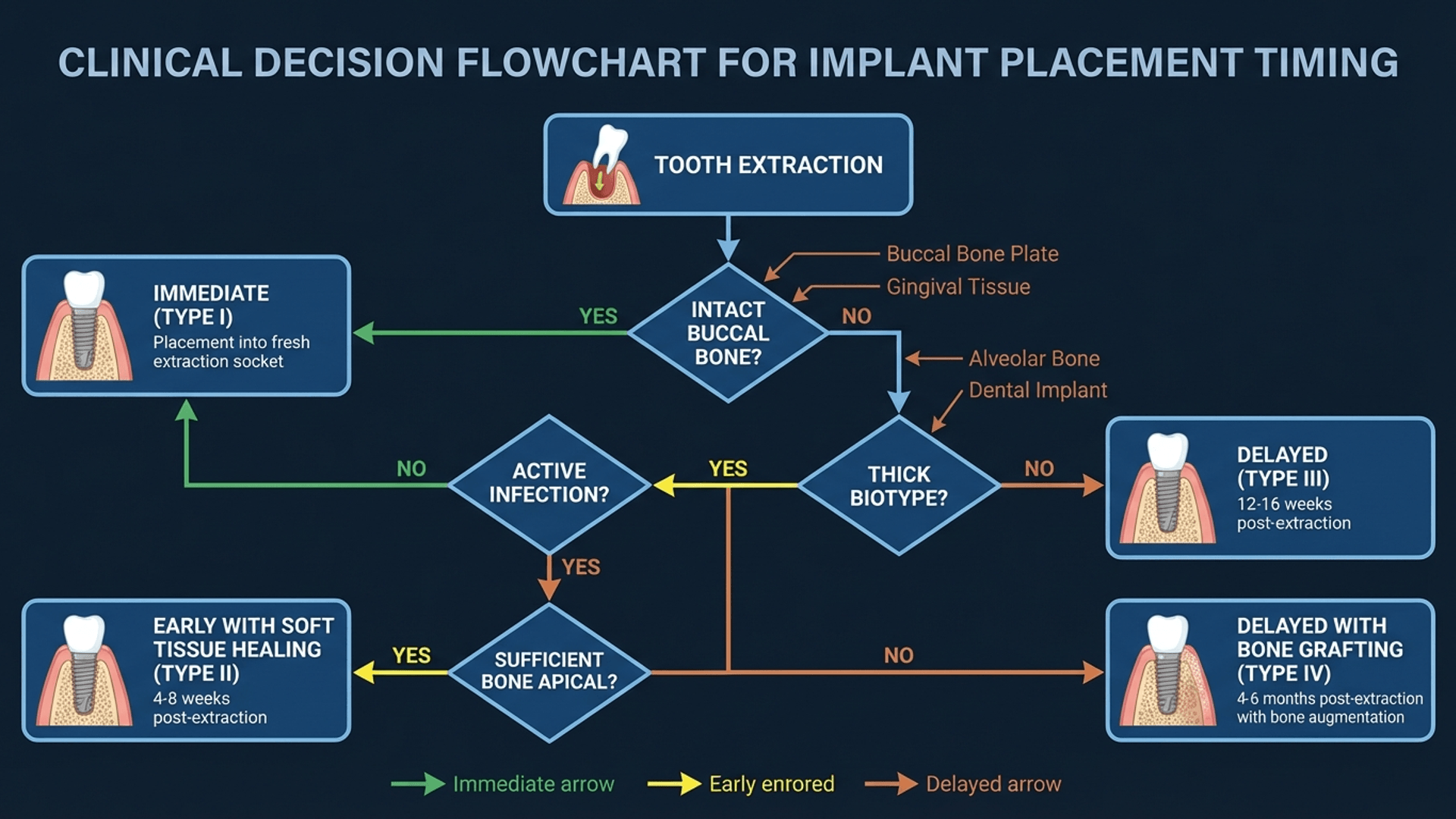
Decision algorithm for selecting optimal implant placement timing (Created with periospot-studio.com)
Choose Immediate Placement (Type I) When:
- Buccal bone wall is intact and >1mm thick
- Thick gingival biotype is present
- No active infection at the site
- Primary stability can be achieved
- Patient has no contraindications (uncontrolled diabetes, heavy smoking, bisphosphonate therapy)
- You have the surgical expertise for this technique-sensitive procedure
Choose Early Placement (Type II/III) When:
- Mild infection requires resolution
- Buccal bone is compromised but regeneration is possible
- Soft tissue needs time to heal for optimal flap management
- The site requires guided bone regeneration
Choose Delayed Placement (Type IV) When:
- Significant bone deficiency requires staged augmentation
- Patient factors preclude earlier intervention
- Complex anatomical situations exist
- You prefer the most predictable, conventional approach
Important: When choosing delayed placement, socket preservation at the time of extraction is critical to maintain ridge volume. Without it, significant bone resorption occurs in the first 3-6 months, potentially complicating the delayed implant procedure.
Loading Protocols: The Next Decision
Once you've determined placement timing, the loading protocol becomes the next critical decision:
Immediate Loading (within 1 week): Requires excellent primary stability (ISQ >70), adequate bone quality, and controlled occlusal forces. The 2025 umbrella review found comparable long-term outcomes between immediate and conventional loading for single implants.
Early Loading (1 week to 2 months): A middle-ground approach that allows some initial healing while reducing treatment time.
Conventional Loading (>2 months): The most established protocol with the longest track record of predictable outcomes.
Technology Integration: Computer-Guided Surgery
The integration of CBCT imaging and computer-guided surgery has transformed immediate implant placement from an art to a science.
Static-guided surgery enables:
- Precise 3D implant positioning
- Flapless approaches that reduce morbidity
- Prosthetically-driven placement
Dynamic navigation offers:
- Real-time adjustments during surgery
- Flexibility for complex anatomical situations
A 2025 systematic review found that both static and dynamic approaches demonstrate superior accuracy compared to freehand placement, with no significant difference between the guided methods.
Complications and How to Avoid Them
Understanding potential complications helps in prevention:
Esthetic Complications
- Gingival recession: Most common with thin biotype; mitigate with connective tissue grafting
- Implant exposure: Result of inadequate palatal positioning or excessive buccal resorption
Biological Complications
- Peri-implant mucositis: Reported in >30% of immediately placed implants in one study
- Peri-implantitis: Risk factors include periodontitis history and smoking
Prevention Strategies
- Rigorous patient selection
- Adequate keratinized mucosa (minimum 2mm)
- Optimal implant positioning
- Appropriate gap management
- Regular maintenance protocols
The Bottom Line: Evidence-Based Decision Making
The 2024-2025 evidence confirms that all implant placement timings can achieve excellent outcomes when properly indicated. The key is matching the timing to the clinical situation and patient factors.
Immediate placement offers reduced treatment time and potential esthetic benefits but requires ideal conditions and surgical expertise. Early placement provides a balanced approach with fewer complications than immediate placement. Delayed placement remains the gold standard for predictability, especially in complex cases.
The most important takeaway: there is no universally "best" timing. The optimal approach is the one that matches the biological reality of the extraction site with the goals of the treatment plan.
As implant dentistry continues to evolve, our decision-making should be guided by evidence rather than tradition. The research is clear—success depends not on when we place the implant, but on whether we've correctly assessed the conditions that favor each timing protocol.
References
Peitsinis PR, et al. Optimizing Implant Placement Timing and Loading Protocols for Successful Functional and Esthetic Outcomes: A Narrative Literature Review. J Clin Med. 2025;14(5):1442.
Riachi E, et al. Clinical Outcomes of Immediate, Early, and Delayed Implant Placement in the Esthetic Zone: A Systematic Review and Meta-analysis. Int J Oral Maxillofac Implants. 2024;39(5):157-173.
Cosyn J, et al. A Systematic Review on Immediate Implant Placement in Intact Versus Non-Intact Alveolar Sockets. J Clin Med. 2025;14(7):2462.
Gareb B, et al. Outcomes of implants placed in sites of previously failed implants: a systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2025;54(3):268-280.
Qian X, et al. Comparison of implant placement and loading protocols for single anterior maxillary implants: A systematic review and network meta-analysis. J Prosthet Dent. 2025;133(3):677-688.
Meta-analysis comparing the outcomes of immediate versus delayed implant placement under periodontitis conditions. ScienceDirect. 2025.
Long-term clinical outcomes of immediate loading versus nonimmediate loading in single-implant restorations: An umbrella review. Dent Res J. 2025;22:41.
Want to create professional dental illustrations like the ones in this article? Visit periospot-studio.com to generate AI-powered clinical diagrams for your presentations and publications.
Comments
0 totalLoading comments...
Previous
How to Build a Dental Portfolio That Actually Opens Doors: A Guide from Someone Who Reviews Them
Next
The 2018 AAP/EFP Periodontal Classification: A Clinician's Complete Guide to Staging and Grading
Related Articles

Machine Learning for Dentists: Predicting Implant Success with AI
1 min read
Socket Preservation: The Complete 2026 Guide to Alveolar Ridge Preservation Techniques
21 min read
