The 2018 AAP/EFP Periodontal Classification: A Clinician's Complete Guide to Staging and Grading

Table of Contents
Marie Kondo became famous for asking one simple question: "Does it spark joy?"
Now, I'm not suggesting you hold each of your patient's teeth and ask if they spark joy before extracting them. But there's something to be learned from the KonMari method about the power of a good classification system.
For decades, we periodontists were like people living in houses with no filing system—shoving papers into drawers, hoping we'd find them later. We had "chronic periodontitis," "aggressive periodontitis," "refractory periodontitis," and a dozen other terms that nobody could agree on. Two clinicians examining the same patient could arrive at completely different diagnoses. It was chaos.
Then, in 2018, the American Academy of Periodontology (AAP) and the European Federation of Periodontology (EFP) got together and basically said: "Enough. Let's KonMari this whole thing."
And thank God they did.
The 2018 classification finally gave us a universal language for periodontal disease. (Created with periospot-studio.com)
Why the Old Classification Needed to Go
The 1999 classification served us for nearly two decades, but it had problems. Big ones.
First, it was built on flimsy scientific foundations. The distinction between "chronic" and "aggressive" periodontitis was based primarily on the rate of disease progression—something we often couldn't determine on a first visit. You'd see a 35-year-old with significant bone loss and think "aggressive periodontitis," when in reality, the disease had been slowly progressing since they were 20 but had never been treated.
Second, the overlap was maddening. Was "aggressive periodontitis" localized or generalized? Was it really different from "early-onset periodontitis" from the 1989 classification? Were we even speaking the same language?
As Tonetti and colleagues (2018) pointed out in the proceedings of the World Workshop:
"The accumulated evidence over 15 years questioned critical elements of the classification system that had been proposed to differentiate the categories."
Translation: We were basically guessing.
The World Workshop of 2018
In November 2017, over 100 experts from around the world gathered in Chicago for the World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. European and American periodontists. Researchers. Clinicians. Everyone who had ever published a paper on periodontitis seemed to be there.
The result? A completely new framework that threw out the old chronic/aggressive distinction and introduced something much more intuitive: Staging and Grading.
If you've ever dealt with cancer staging (and I hope you haven't personally), this will feel familiar. It's the same logic oncologists use—and it works beautifully for periodontitis.
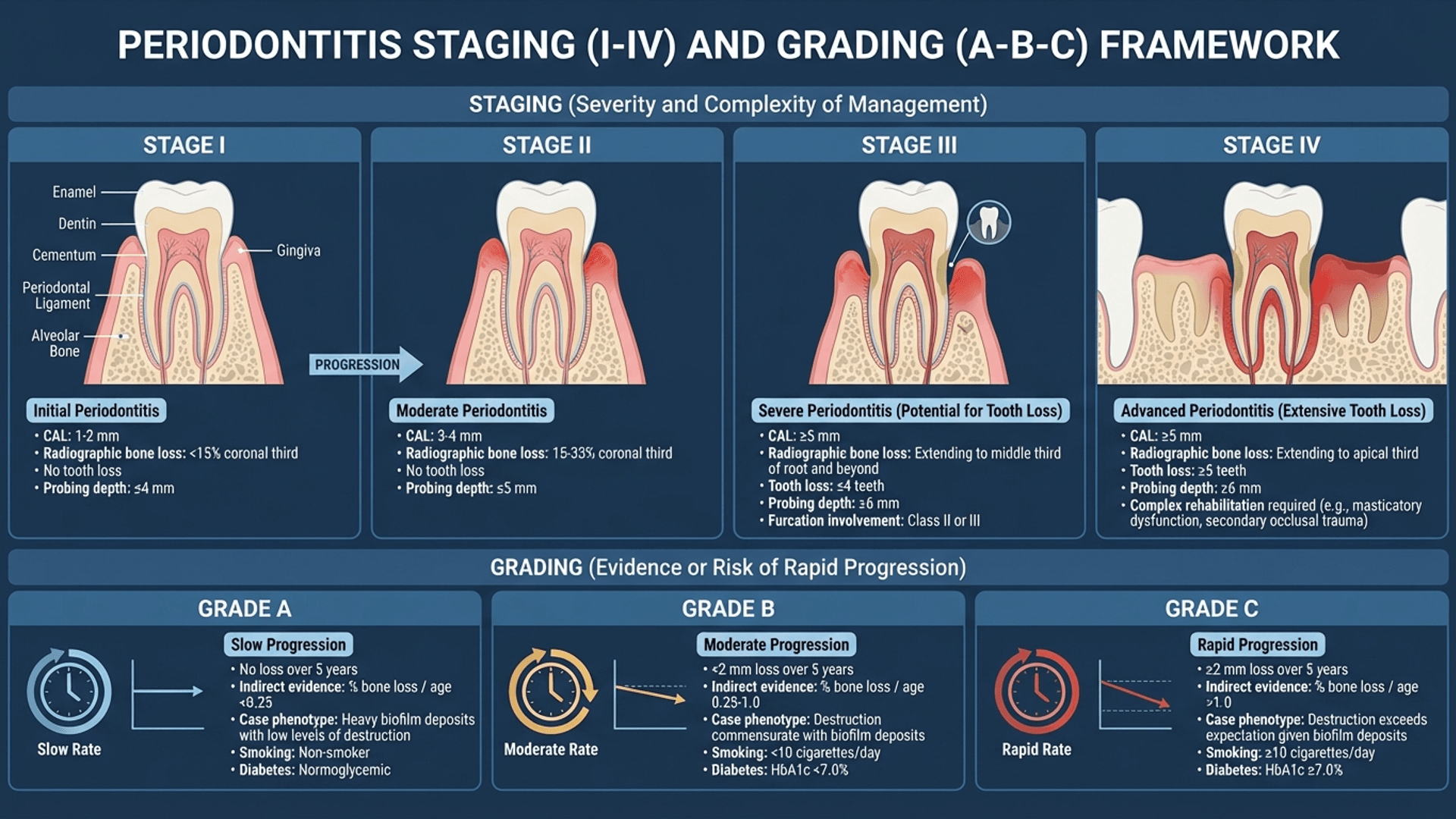
Understanding Staging: How Bad Is It Right Now?
Staging tells you the severity and complexity of the disease. It answers the question: "How much damage has been done?"
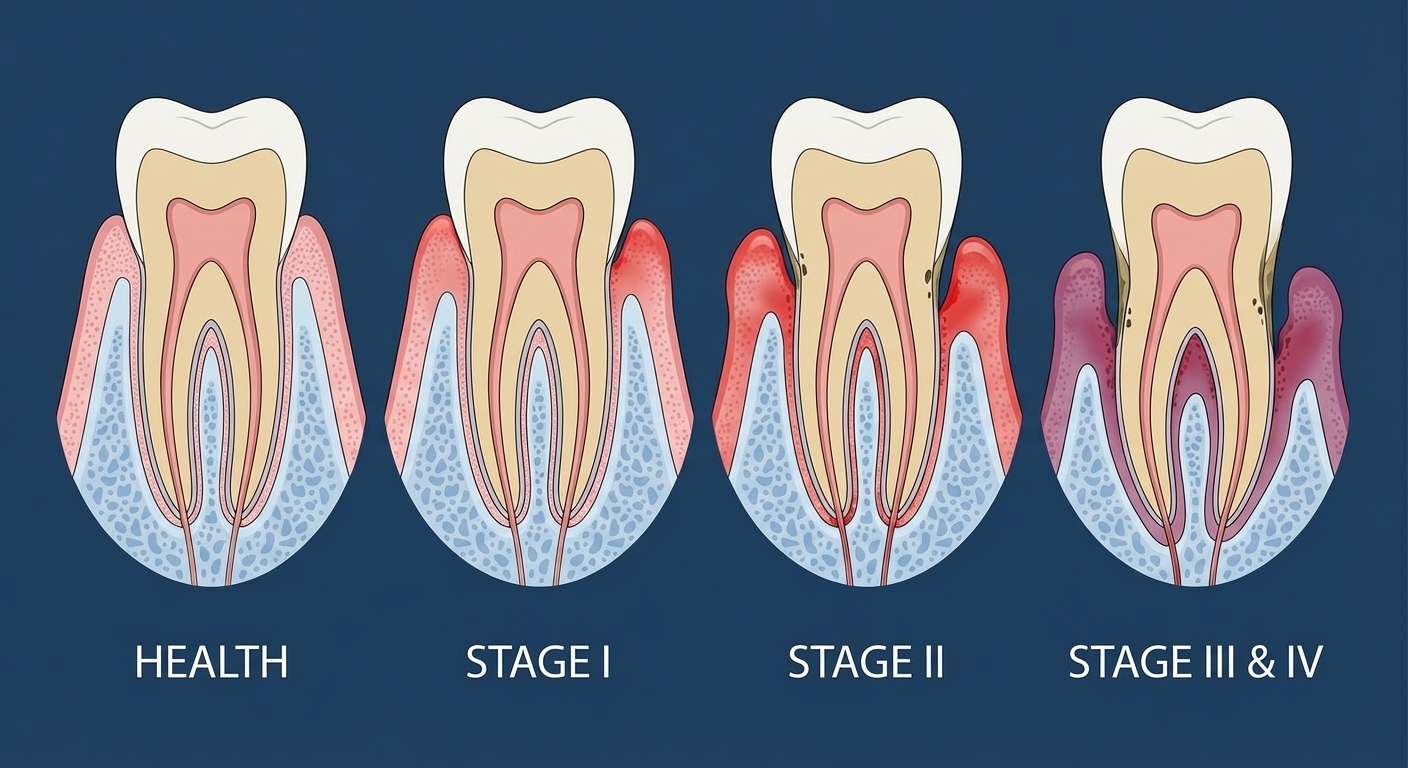
The four stages of periodontitis based on severity and complexity. (Created with periospot-studio.com)
Stage I: Initial Periodontitis
This is where you catch it early—if you're paying attention during perio charting.
The defining features:
- Clinical attachment loss (CAL): 1-2 mm
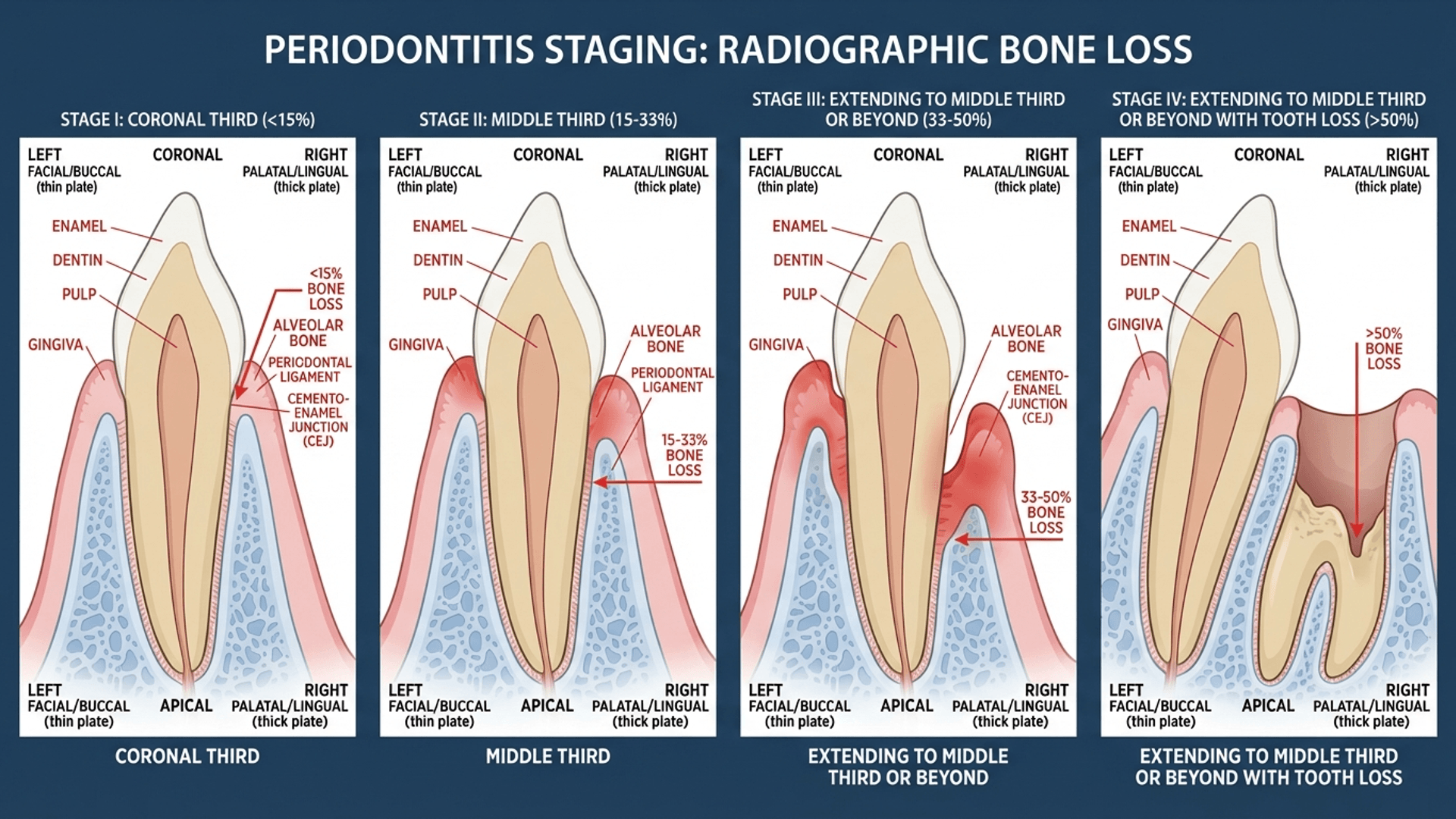
- Radiographic bone loss: Coronal third of the root (<15%)
- Probing depths: Maximum 4 mm
- No tooth loss due to periodontitis
This is the patient who shows up with a few 4 mm pockets, some bleeding on probing, but nothing scary on the radiographs. You can manage this without referral. Scaling, root planing, good home care, and they're usually golden.
Stage II: Moderate Periodontitis
Now we're getting into territory where you need to be more careful.
The defining features:
- CAL: 3-4 mm
- Radiographic bone loss: Coronal third (15-33%)
- Probing depths: Maximum 5 mm
- No tooth loss due to periodontitis
The bone loss is more visible now. Still manageable with non-surgical therapy in most cases, but you're watching these patients more closely. This is the stage where good perio charting habits pay off—catch the progression early, intervene appropriately.
Stage III: Severe Periodontitis with Potential for Tooth Loss
Here's where things get serious.
The defining features:
- CAL: ≥5 mm
- Radiographic bone loss: Extending to middle third of root or beyond
- Probing depths: ≥6 mm
- Tooth loss: ≤4 teeth due to periodontitis
Complexity factors that can bump you to Stage III:
- Vertical bone loss ≥3 mm
- Furcation involvement Class II or III
- Moderate ridge defects
This patient needs more than scaling. You're looking at surgical intervention, regenerative procedures, potential extractions. If you're a general dentist, this is where you seriously consider referral.
Stage IV: Advanced Periodontitis with Extensive Tooth Loss
The bad news stage.
The defining features:
- Everything from Stage III, plus:
- Tooth loss: ≥5 teeth due to periodontitis
- Masticatory dysfunction
- Secondary occlusal trauma
- Severe ridge defects
- Bite collapse, drifting, flaring
Stage IV isn't just about periodontitis anymore—it's about rehabilitation. You're dealing with functional problems that require complex treatment planning involving prosthodontics, possibly orthodontics, and significant time and resources.
Staging defines severity while grading defines progression rate. (Created with periospot-studio.com)
Understanding Grading: How Fast Is It Progressing?
Here's where the 2018 classification really shines. Staging tells you how bad things are NOW. Grading tells you how FAST the disease is likely to progress.
This is crucial information. Two patients can both have Stage III periodontitis, but if one is Grade A (slow progression) and the other is Grade C (rapid progression), your treatment approach and prognosis are completely different.
Grade A: Slow Progression
The profile:
- Bone loss / age ratio: <0.25
- Heavy biofilm deposits with low destruction levels
- No bone loss over 5 years (if longitudinal data available)
- Non-smoker, no diabetes
This is the patient who's had periodontitis for 30 years but still has most of their teeth. The disease is there, but it's moving slowly. With proper management, they can keep their teeth for a long time.
Grade B: Moderate Progression
The profile:
- Bone loss / age ratio: 0.25 to 1.0
- Destruction commensurate with biofilm deposits
- Less than 2 mm bone loss over 5 years
- Smoker (<10 cigarettes/day) or HbA1c <7% in diabetics
This is your "typical" periodontitis patient. The disease is progressing at a moderate rate, and they need consistent maintenance and monitoring.
Grade C: Rapid Progression
The profile:
- Bone loss / age ratio: >1.0
- Destruction exceeds what you'd expect from biofilm
- More than 2 mm bone loss over 5 years
- Heavy smoker (≥10 cigarettes/day) or HbA1c ≥7% in diabetics
This is the 35-year-old with bone loss that looks like a 60-year-old's. The disease is aggressive. These patients need intensive treatment and very close monitoring.
The Bone Loss / Age Ratio: A Practical Tool
One of the best additions in the 2018 classification is the bone loss / age ratio. It's simple math that gives you incredible insight.
How to calculate it:
- Measure the worst site's bone loss as a percentage of root length
- Divide by the patient's age
Example:
A 40-year-old patient with 50% bone loss at the worst site.
Ratio = 50/40 = 1.25
That's Grade C territory—rapid progression.
A 70-year-old patient with 40% bone loss at the worst site.
Ratio = 40/70 = 0.57
That's Grade B—moderate progression.
Same amount of bone loss, but completely different disease behaviors. This is why the grading system is so powerful.
Practical Perio Charting: Putting It All Together
Alright, let's get practical. How do you actually use this in daily clinical practice?
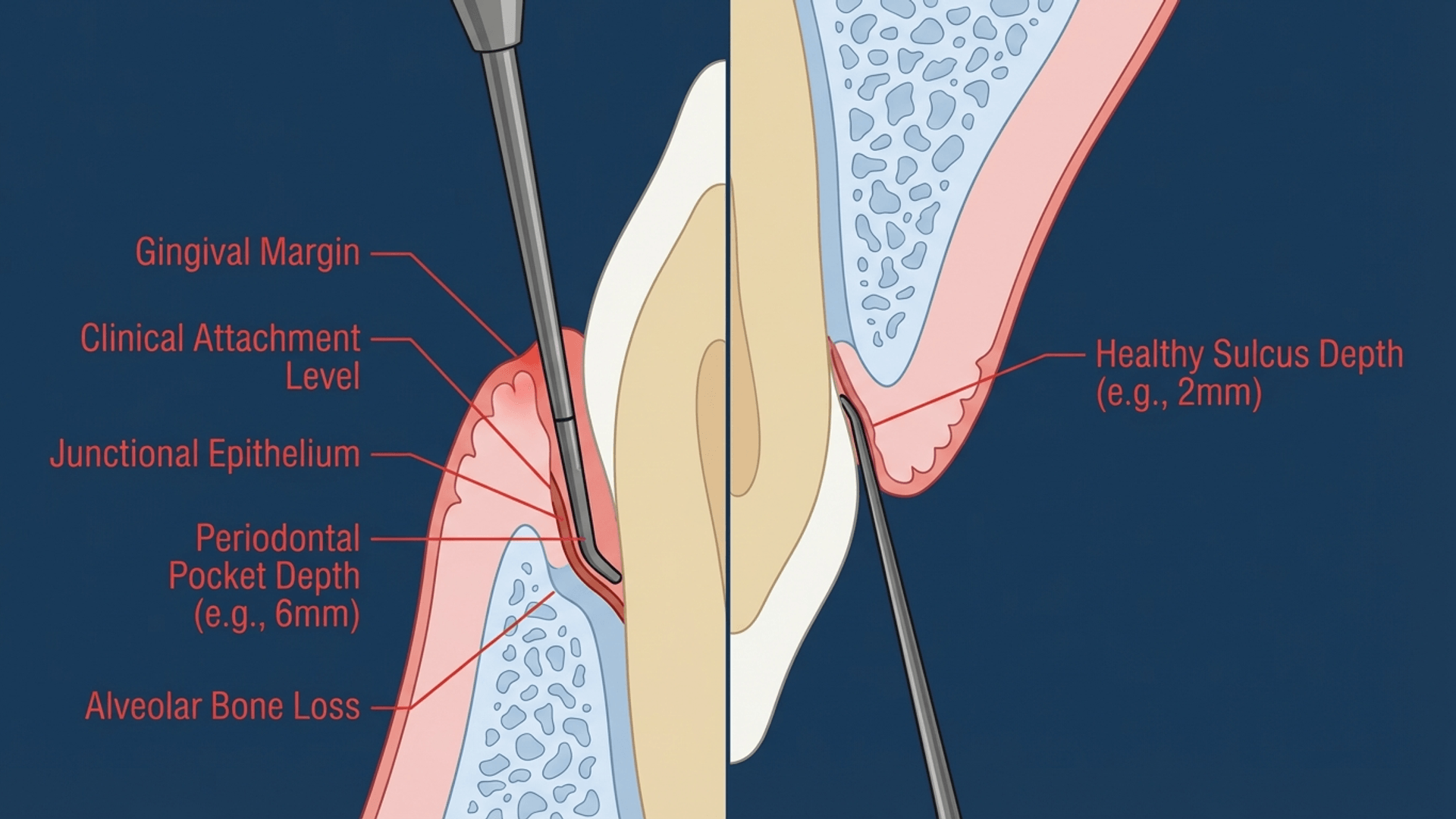
Accurate periodontal probing is the foundation of proper classification. (Created with periospot-studio.com)
Step 1: Complete Periodontal Examination
You can't classify what you don't measure. This means:
- Full-mouth probing (6 sites per tooth, minimum)
- Bleeding on probing assessment
- Recession measurements
- Furcation assessment on all molars
- Full-mouth radiographic series
Don't cut corners here. A bite-wing series won't show you interproximal bone loss on posterior teeth. You need periapicals or a CBCT for complex cases.
Step 2: Calculate Clinical Attachment Loss
Remember, CAL = Probing Depth + Recession
If the gingival margin is coronal to the CEJ, you subtract that distance from the probing depth. If it's apical (recession), you add it.
This is the number that drives staging. Probing depths alone can be misleading—a 4 mm pocket with 2 mm of recession is actually 6 mm of CAL.
Step 3: Assess Radiographic Bone Loss
Look at your radiographs and estimate the percentage of root length with bone loss. The coronal third, middle third, and apical third each represent roughly 33%.
Pro tip: Use the CEJ to the root apex as your reference. Measure from where the bone should be (2 mm below CEJ) to where it actually is.
Step 4: Identify Complexity Factors
Check for:
- Furcation involvement (especially Class II and III)
- Vertical bone defects
- Tooth mobility and secondary occlusal trauma
- Ridge defects
- Number of teeth lost to periodontitis
These factors can bump a patient from one stage to the next, regardless of the primary criteria.
Step 5: Determine Grade
Look at:
- Age of the patient
- Amount of bone loss
- Available longitudinal data (if any)
- Risk factors (smoking, diabetes)
When in doubt between grades, choose the higher one. It's better to be more aggressive with treatment than to underestimate disease progression.
Step 6: Document Everything
Your perio chart should include:
- Stage (I, II, III, or IV)
- Grade (A, B, or C)
- Extent (localized <30% of teeth or generalized ≥30%)
- Distribution pattern (molar-incisor pattern if applicable)
A complete diagnosis might read: "Stage III, Grade C, Generalized Periodontitis" or "Stage II, Grade B, Localized Periodontitis."
The Extent and Distribution Descriptors
The 2018 classification also clarified how we describe the extent and distribution of periodontitis:
Extent:
- Localized: <30% of teeth affected
- Generalized: ≥30% of teeth affected
Distribution:
- Molar-incisor pattern: A specific pattern primarily affecting first molars and incisors (the old "localized aggressive periodontitis" pattern)
Risk Factor Modification in the New System
One aspect I particularly appreciate is how the 2018 classification handles risk factors. Smoking and diabetes aren't just clinical notes anymore—they directly influence the grade.
This forces us to have conversations with patients about systemic health. "Mrs. Johnson, your periodontitis is progressing rapidly—partly because of your uncontrolled diabetes. We need to work with your physician to get your HbA1c below 7%."
That's powerful. The classification system becomes a communication tool.
Common Mistakes to Avoid
After teaching this classification for several years, I've noticed some recurring errors:
1. Staging based on probing depth alone
Probing depth is important, but CAL and radiographic bone loss drive staging. A 3 mm pocket with 4 mm of recession is Stage II or III, not Stage I.
2. Ignoring complexity factors
A patient with 4 mm CAL but Class III furcation involvement is Stage III, not Stage II. The complexity factors matter.
3. Not calculating the bone loss/age ratio
This is such a simple calculation that gives you so much information. Don't skip it.
4. Defaulting to Grade B
When you're unsure, you're supposed to assume Grade B. But don't let this become a lazy default. Actually calculate the ratio and assess risk factors.
5. Forgetting about extent
The extent (localized vs. generalized) is part of the complete diagnosis. Include it.
Why This Classification Actually Matters for Your Patients
At this point, you might be thinking: "Great, another classification system to memorize. How does this actually help my patients?"
Here's the thing—the 2018 classification isn't just academic navel-gazing. It changes how we treat patients.
For Stage I patients: We can confidently manage them with non-surgical therapy and regular maintenance, knowing that with proper care, they're unlikely to progress.
For Stage III Grade C patients: We know aggressive intervention is needed NOW, not after three more years of "watchful waiting."
For diabetic patients: The direct incorporation of HbA1c into grading means we're forced to coordinate care with their physicians.
For smokers: The grading system gives us concrete evidence to show patients how smoking accelerates their disease.
The classification is a communication tool between clinicians, between you and your patients, and between you and insurance companies trying to deny coverage.
Conclusion: Embrace the Change
I'll admit, when the 2018 classification first came out, I was skeptical. "Another classification system? Didn't we just learn the last one?"
But after using it in practice for years, I'm a convert. The staging and grading system just makes sense. It's intuitive, it's clinically useful, and it gives us a common language that transcends continents and practice settings.
Is it perfect? No. There are still gray areas and room for interpretation. But compared to the confusion of "chronic versus aggressive periodontitis," this is a massive improvement.
So next time you're doing your perio charting, think about Marie Kondo. Does this tooth spark joy? No? That's okay—let's stage and grade its periodontitis properly, and figure out how to keep it around a bit longer.
📚 Recommended Reading
If you want to go deeper into periodontal classification and clinical periodontology, there's really only one book you need on your shelf:
Clinical Periodontology and Implant Dentistry (7th Edition) by Jan Lindhe, Niklaus P. Lang, and Tord Berglundh
This two-volume set is the bible of periodontology. The 7th edition includes comprehensive coverage of the 2018 classification system, with detailed chapters on staging, grading, and the scientific rationale behind the changes. It's not cheap, but it's the reference you'll use for your entire career.
Get it on Amazon (affiliate link)
References:
Caton JG, Armitage G, Berglundh T, et al. A new classification scheme for periodontal and peri-implant diseases and conditions – Introduction and key changes from the 1999 classification. J Clin Periodontol. 2018;45 Suppl 20:S1-S8.
Tonetti MS, Greenwell H, Kornman KS. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J Clin Periodontol. 2018;45 Suppl 20:S149-S161.
Papapanou PN, Sanz M, Buduneli N, et al. Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Clin Periodontol. 2018;45 Suppl 20:S162-S170.
Herrera D, Figuero E, Shapira L, Jin L, Sanz M. La nueva clasificación de las enfermedades periodontales y periimplantarias. Revista Científica de la Sociedad Española de Periodoncia. 2018;4(11):94-110.
Lindhe J, Lang NP. Clinical Periodontology and Implant Dentistry. 7th ed. Wiley-Blackwell; 2022.
Want to create professional dental illustrations like the ones in this article? Visit periospot-studio.com to learn how AI can transform your dental education content.
Do you have questions about applying the 2018 classification in your practice? Leave a comment below—I'd love to hear about the challenging cases you're encountering.
Comments
0 totalLoading comments...
Previous
Immediate Implant Placement: The 2025 Evidence-Based Guide for Clinical Success
Next
Osseointegration: The Stuff That Actually Makes Dental Implants Work (And Why You Should Care)
Related Articles

Machine Learning for Dentists: Predicting Implant Success with AI
1 min read
Osseointegration: The Stuff That Actually Makes Dental Implants Work (And Why You Should Care)
13 min read