Bundle Bone: The Complete Guide to Gap Management & Immediate Implants [2025 Update]
![Bundle Bone: The Complete Guide to Gap Management & Immediate Implants [2025 Update]](/_next/image?url=https%3A%2F%2Fajueupqlrodkhfgkegnx.supabase.co%2Fstorage%2Fv1%2Fobject%2Fpublic%2Fimages%2Fposts%2Fbundle-bone-the-complete-guide-to-gap-management-immediate-implants%2Fregenerated-1768916026108.jpeg&w=2048&q=75)
Table of Contents
It was 2004 when Chen and colleagues published their landmark study on immediate implant placement. A year later, Araújo and Lindhe would shake the implant world with findings that challenged everything we thought we knew about socket healing. Two decades later, the debate continues—but now we have answers.
The bundle bone. Two words that separate the implant dentists who achieve predictable aesthetic results from those who don't. Understanding this thin layer of tooth-dependent bone is not optional—it's fundamental to every decision you make in the anterior zone.
In this comprehensive guide, I'll walk you through 12 critical facts about bundle bone, gap management, and immediate implant protocols. These aren't theoretical concepts—they're the principles I've applied in thousands of cases over 30 years of clinical practice.
Whether you're planning your first immediate implant or refining protocols you've used for years, this guide will give you the biological foundation and clinical frameworks to make better decisions.
What Is Bundle Bone? The Foundation You Must Understand
Before we dive into the 12 facts, let's establish what we're actually talking about.
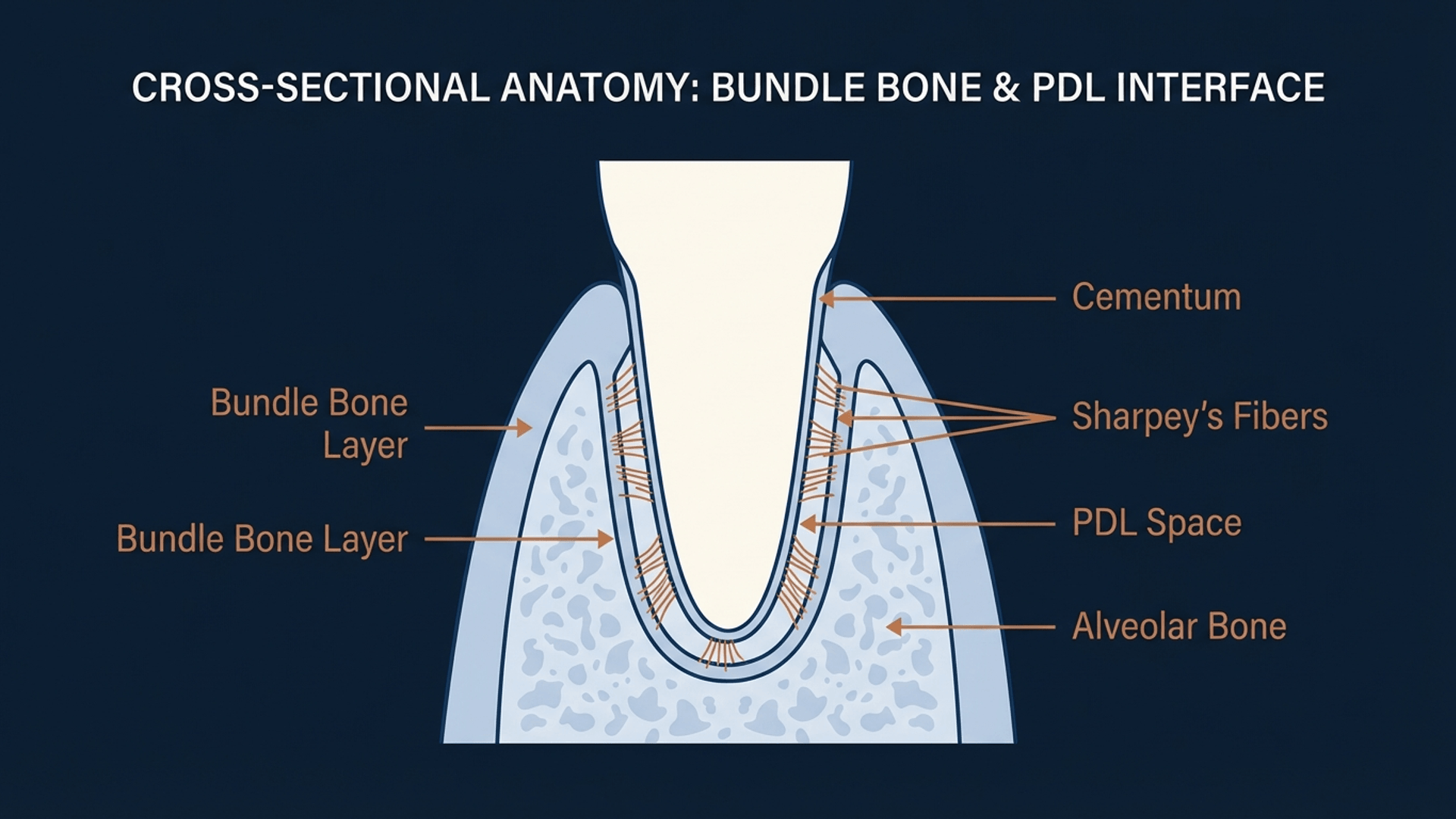
Bundle bone (also called alveolar bone proper or cribriform plate) is the thin layer of bone that lines the tooth socket. It's characterized by the insertion of Sharpey's fibers from the periodontal ligament—making it fundamentally tooth-dependent tissue.
[Image generated with Periospot Studio]
Here's the critical point: Bundle bone cannot exist without a tooth.
The moment you extract a tooth, you don't just remove enamel, dentin, and pulp. You remove the entire periodontal apparatus—and with it, the blood supply that maintains the bundle bone. What follows is inevitable resorption.
This isn't a defect. It's biology. And until you internalize this concept, you'll continue to be surprised by post-extraction ridge changes.
Bundle Bone, Lamina Dura & Alveolar Bone Proper: Same Structure, Different Perspectives
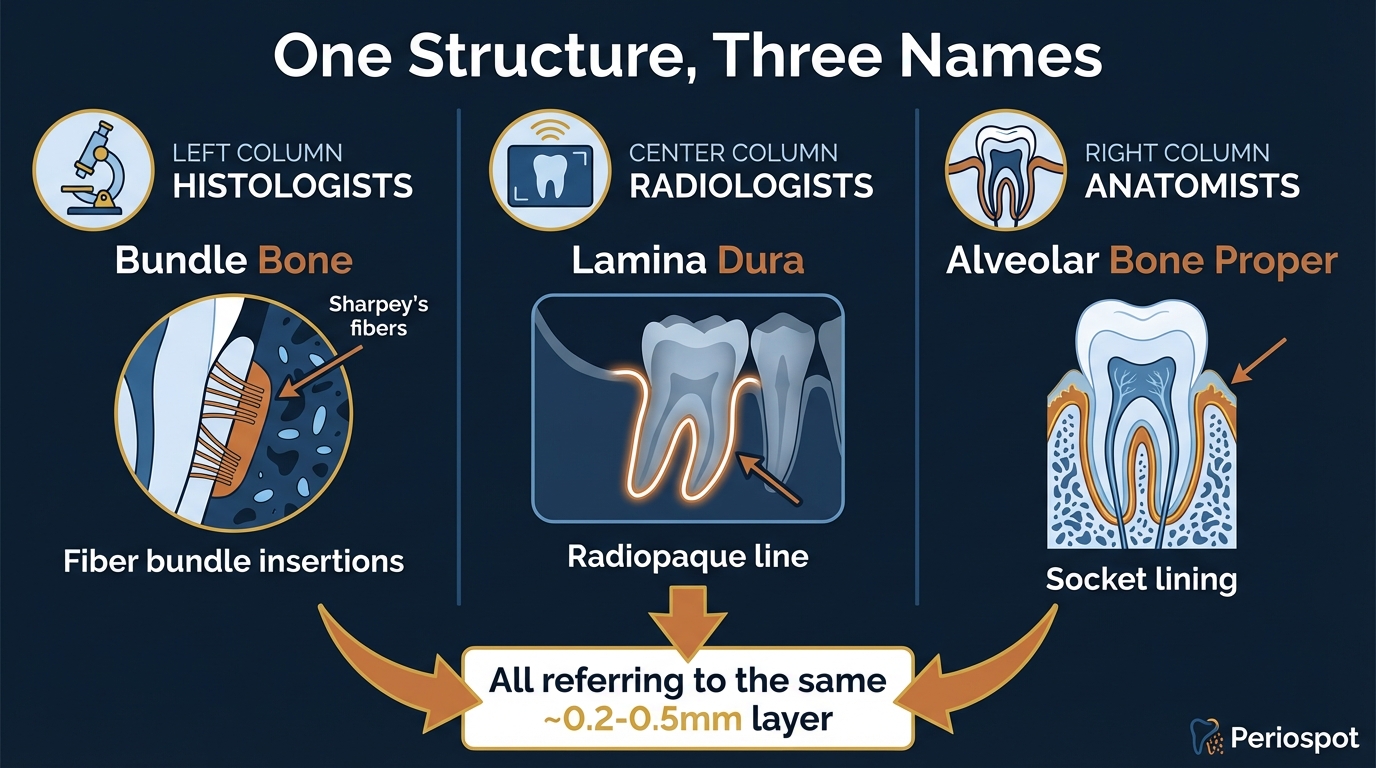
Here's something that confuses even experienced clinicians: bundle bone, lamina dura, and alveolar bone proper are actually the same anatomical structure—just named differently depending on who's looking at it and how.
[Image generated with Periospot Studio]
Why Three Names for One Structure?
| Who Uses the Term | What They Call It | How They See It | Key Feature |
|---|---|---|---|
| Histologists | Bundle Bone | Under the microscope | Sharpey's fiber insertions creating "bundles" |
| Radiologists | Lamina Dura | On X-rays/CBCT | Dense white line surrounding tooth roots |
| Anatomists | Alveolar Bone Proper | In dissection/textbooks | Thin bone layer lining the tooth socket |
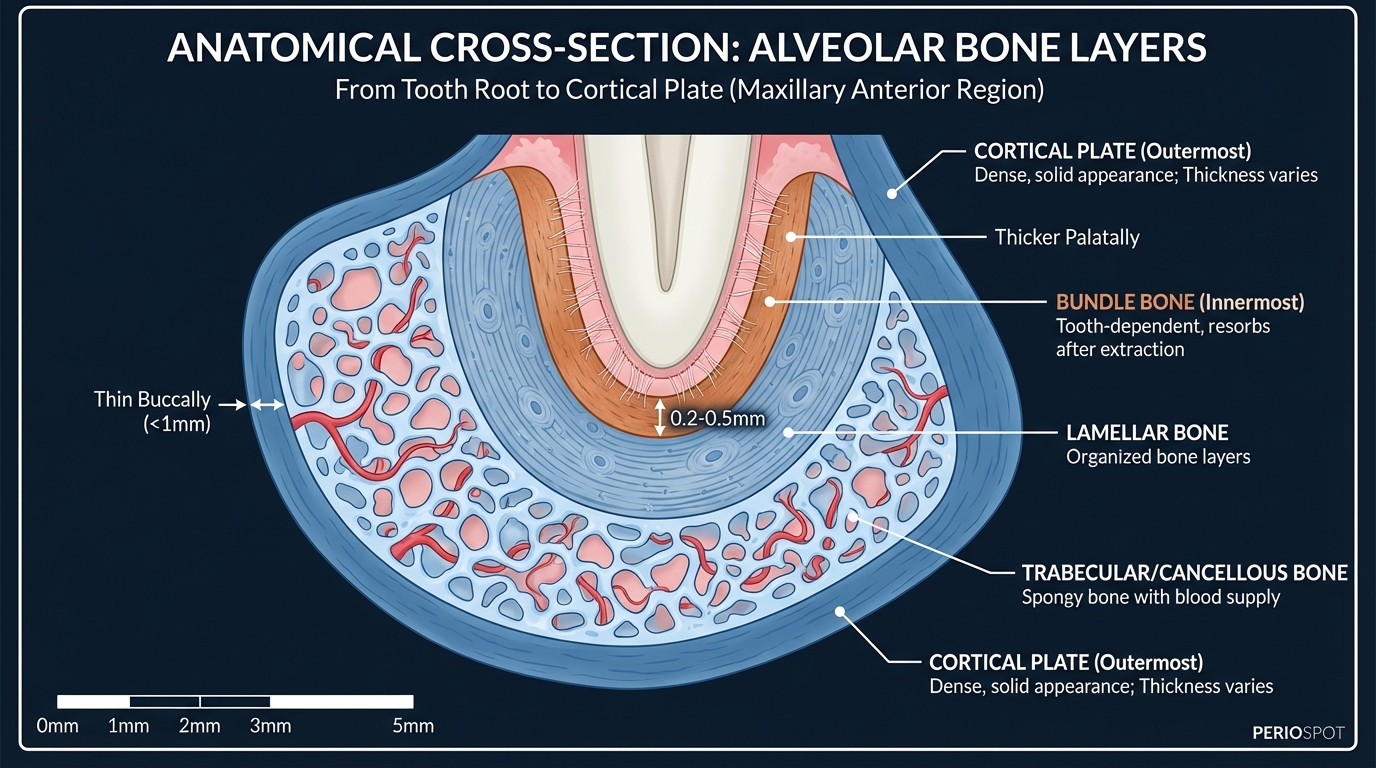
Understanding the Four Layers of Alveolar Bone
To truly understand bundle bone, you need to visualize where it fits in the larger picture. The alveolar process consists of four distinct layers:
[Image generated with Periospot Studio]
| Layer | Thickness | Characteristics | Clinical Significance |
|---|---|---|---|
| Bundle Bone | 0.2-0.5mm | Sharpey's fibers, tooth-dependent | Resorbs after extraction |
| Lamellar Bone | Variable | Organized concentric layers | Provides structural support |
| Trabecular Bone | Variable | Spongy, contains marrow spaces | Houses blood supply |
| Cortical Plate | <1mm buccally | Dense outer shell | Protection |
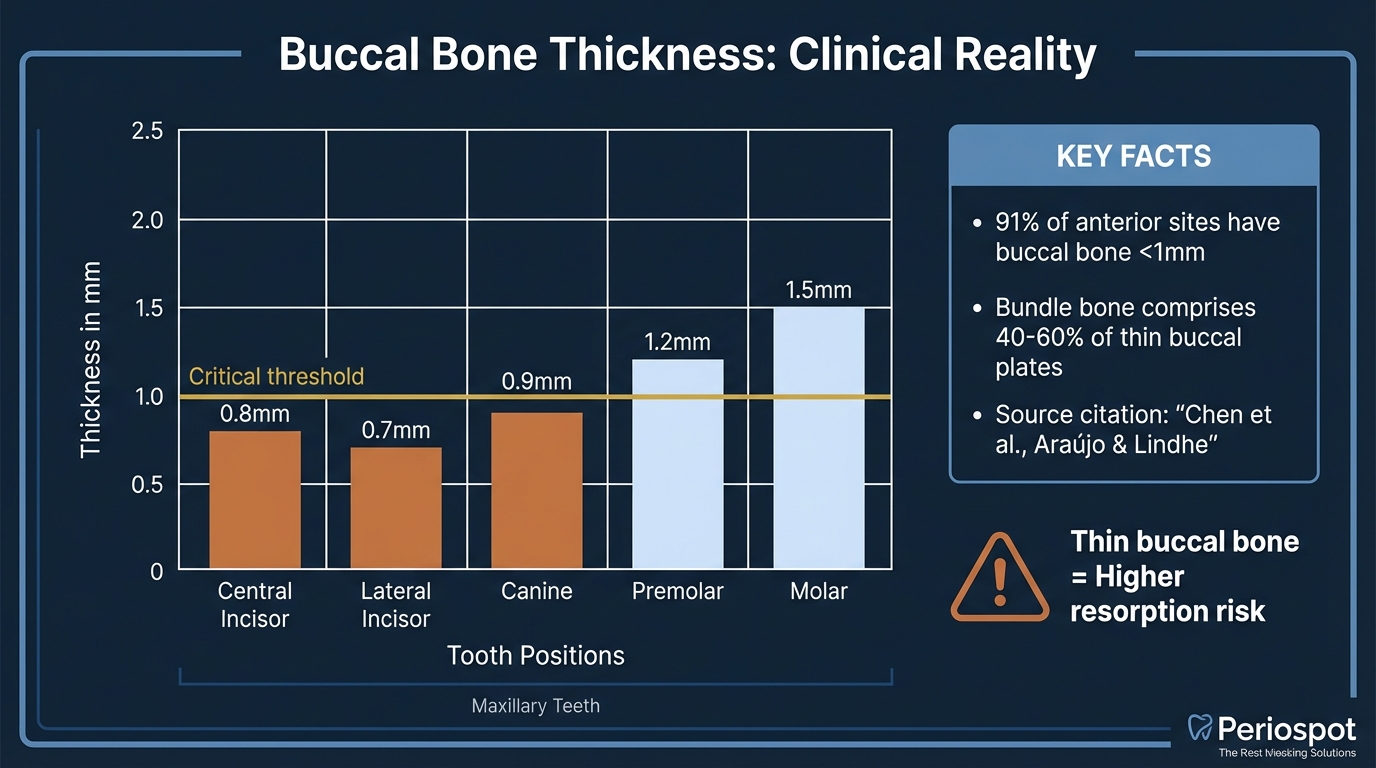
Clinical Reality: Buccal Bone Thickness Data
The buccal bone in the anterior maxilla is remarkably thin—often much thinner than clinicians expect. This has profound implications for immediate implant placement:
[Image generated with Periospot Studio]
Key findings from clinical studies:
- 91% of anterior maxillary sites have buccal bone <1mm
- Bundle bone comprises 40-60% of thin buccal plates
- Central and lateral incisors have the thinnest buccal bone
The Resorption Timeline: What Happens After Extraction
Once you understand that bundle bone is tooth-dependent, the post-extraction timeline becomes predictable:
[Image generated with Periospot Studio]
The Clinical Takeaway: Whether you call it bundle bone, lamina dura, or alveolar bone proper, the biology is the same—this thin layer of tooth-dependent bone will resorb once the tooth is removed. Your protocol decisions should be based on this fundamental understanding.
Histological Composition of Bundle Bone
Bundle bone consists of:
- Lamellar bone with distinctive Sharpey's fiber insertions
- Rich vascular network supplied by the periodontal ligament
- Thickness of approximately 0.2-0.4mm on the buccal aspect
The buccal plate in the anterior maxilla is often paper-thin—sometimes less than 1mm total thickness, with bundle bone comprising a significant portion.
The 12 Facts: Clinical Insights That Change Practice
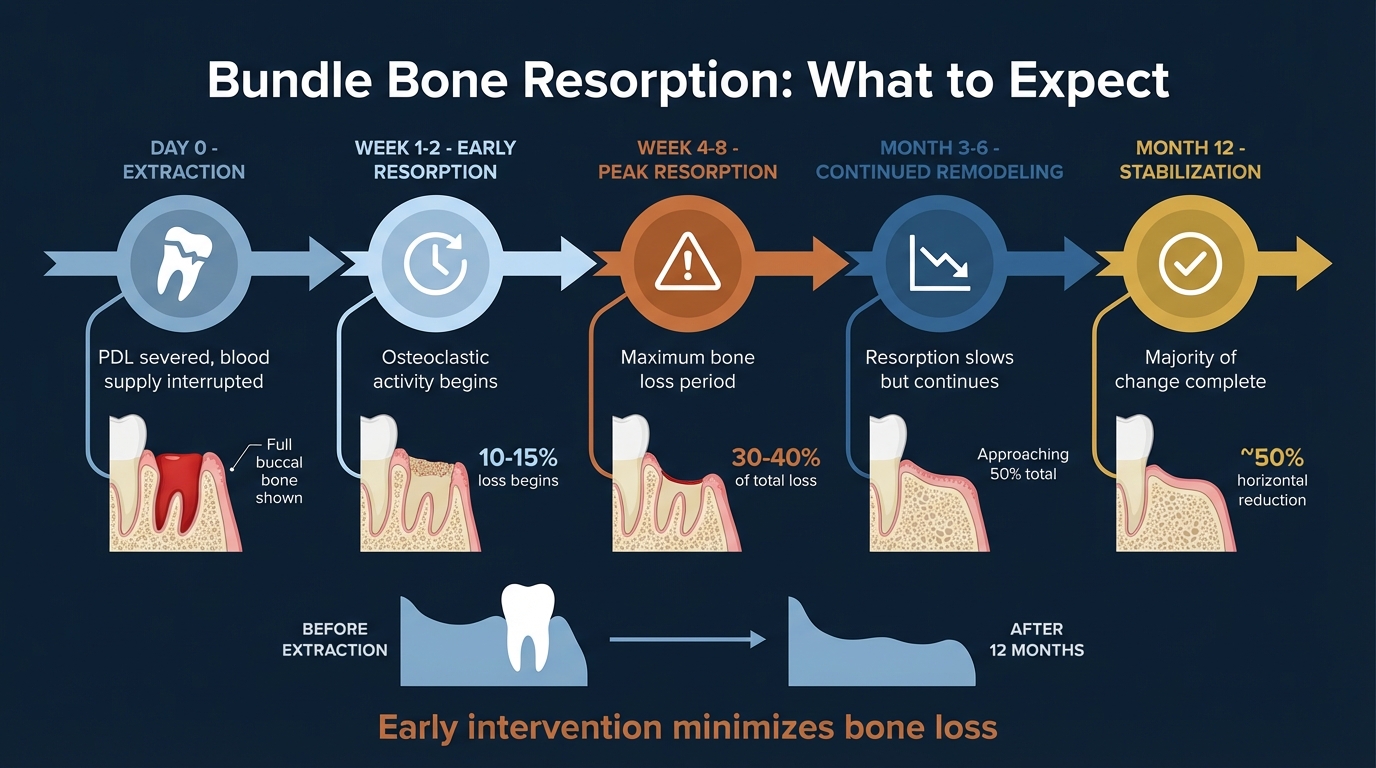
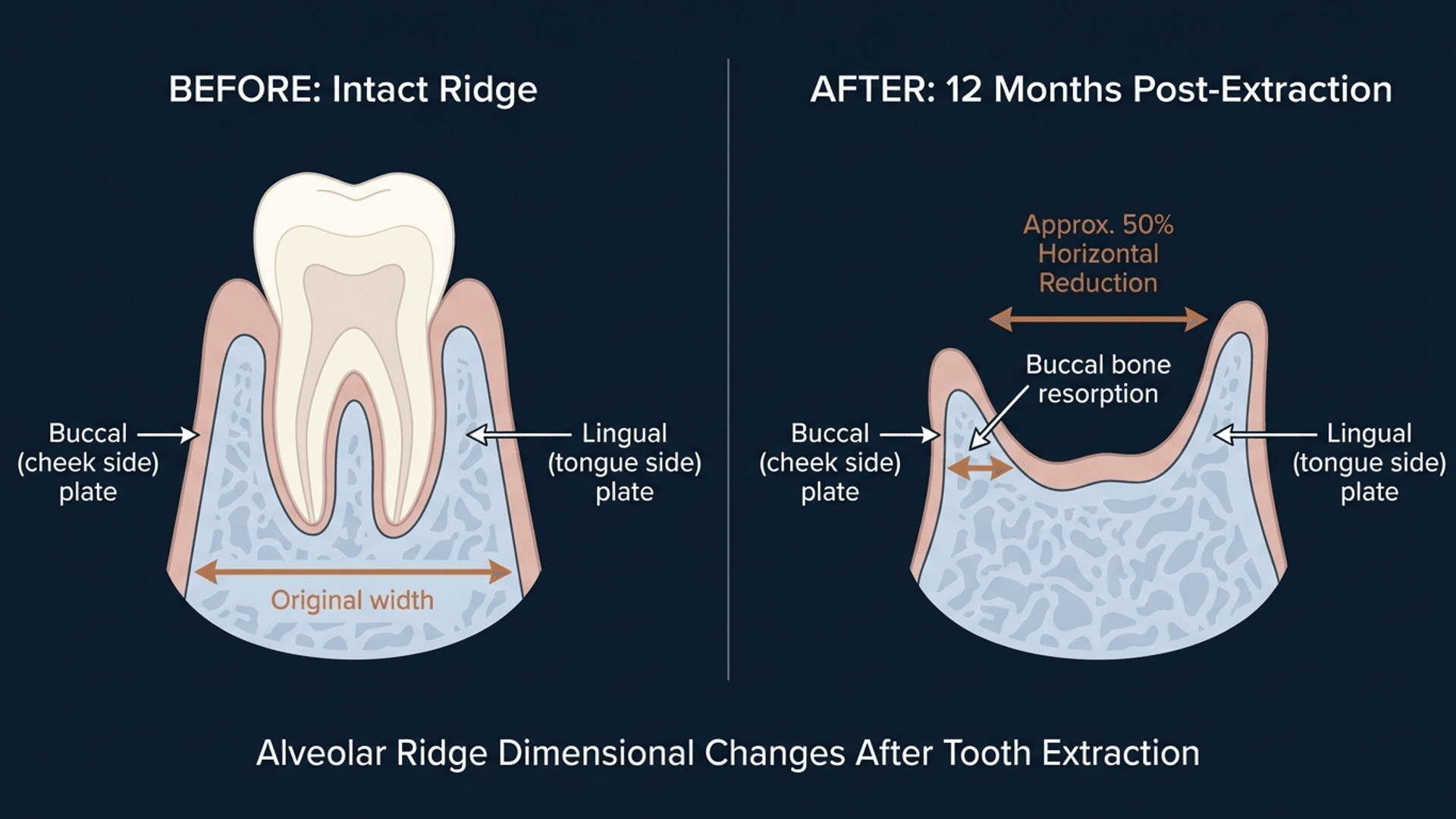
Fact 1: Extraction Causes 50% Buccal Width Reduction
The science: After tooth extraction, the alveolar ridge undergoes dramatic dimensional changes. Multiple systematic reviews confirm approximately 50% horizontal reduction occurs within the first 12 months, with the majority happening in the first 3 months.
[Image generated with Periospot Studio]
Why it matters clinically: That beautiful, full buccal contour you see at extraction? Assume half of it will disappear. This isn't pessimism—it's planning reality.
The buccal bone resorbs more than the palatal/lingual bone because:
- The buccal plate is thinner
- It contains proportionally more bundle bone
- It has less trabecular bone support
Clinical takeaway: When evaluating extraction sites for immediate placement, measure the buccal bone thickness. If it's less than 1mm (which it often is in the anterior maxilla), expect significant resorption regardless of your protocol.
Fact 2: Loss of Periodontal Ligament Means No More Blood Supply
The science: The periodontal ligament (PDL) isn't just an attachment apparatus—it's a vascular highway. The PDL provides approximately 70% of the blood supply to the bundle bone.
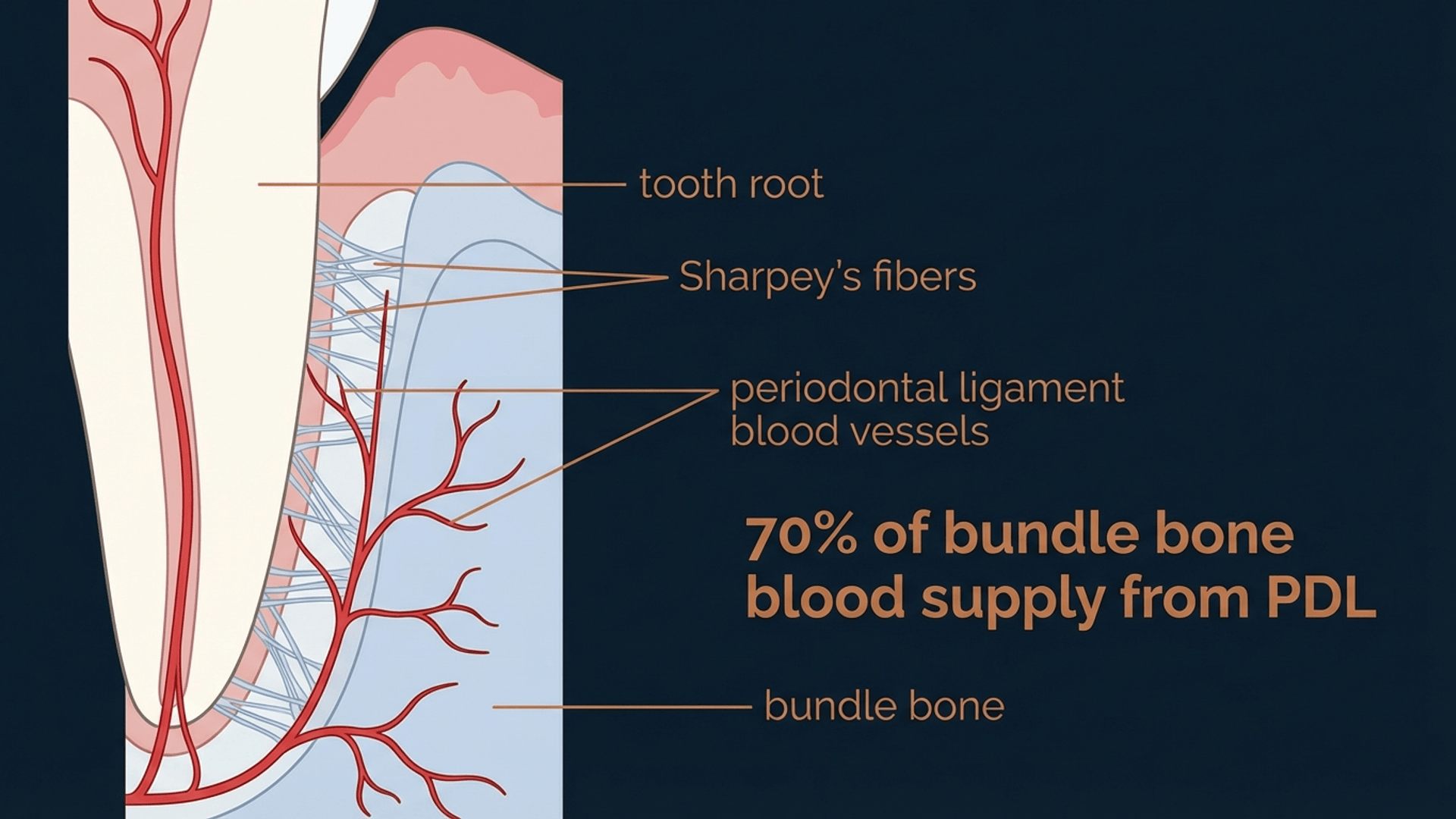
[Image generated with Periospot Studio]
When you extract a tooth, you sever this blood supply instantly. The bundle bone, now devoid of its primary vascular source, begins to resorb.
The resorption cascade:
- Day 0: PDL severed, blood supply interrupted
- Week 1-2: Osteoclastic activity begins
- Week 4-8: Peak resorption period
- Month 3-6: Remodeling continues but slows
- Month 12: Majority of dimensional change complete
Why this matters: No technique, no biomaterial, and no implant design can fully compensate for this biological reality. The best we can do is manage the resorption—not prevent it entirely.
Clinical takeaway: Time is not your friend after extraction. Every week you wait, you lose hard and soft tissue volume. This is why the timing debate (immediate vs. delayed) matters so much.
Fact 3: Immediate Implants Have a Direct Relationship with Buccal Bone Loss
The science: Here's where it gets controversial. Early advocates of immediate implants believed that placing an implant into a fresh socket would "maintain" the buccal bone.
They were wrong.
Chen et al. (2004) and Araújo et al. (2005, 2006) demonstrated that immediate implant placement does NOT prevent bundle bone resorption. The buccal bone resorbs regardless of implant presence.
In fact, some studies suggest the resorption pattern may be similar whether you place an implant or not—the bundle bone simply cannot survive without the tooth.
The nuance: This doesn't mean immediate implants are bad. It means we need to set appropriate expectations and plan for the resorption that WILL occur.
Clinical takeaway: Don't promise patients that immediate implants will "preserve" their bone. Instead, explain that immediate placement offers advantages in treatment time and soft tissue preservation—while acknowledging that some buccal contour change is inevitable.
Fact 4: Implants Do NOT Preserve Alveolar Bone
The science: This fact reinforces and expands on Fact 3. Let me be direct: implants are not bone-preserving devices.
An implant is a prosthetic anchor. It integrates with bone (osseointegration), but it does not replicate the biological functions of a tooth root. Specifically:
- No periodontal ligament
- No Sharpey's fibers
- No proprioception
- No dynamic bone stimulation through PDL
The bone around an implant remodels according to different biological rules than bone around teeth.
Why this matters: The marketing message that "implants preserve bone" is misleading. Implants prevent the continued resorption you'd see in an edentulous ridge, but they don't preserve the original bone volume present at extraction.
Clinical takeaway: Separate "maintaining what remains" from "preserving what was." Implants do the former, not the latter. Plan your cases accordingly.
Fact 5: Ridge Preservation Is Almost Always a Better Option
The science: If immediate implants don't prevent bone loss, what does? Ridge preservation procedures can significantly reduce dimensional changes after extraction.
Socket grafting with various biomaterials (xenografts, allografts, synthetics) combined with membrane coverage has been shown to:
- Reduce horizontal resorption by 1-2mm compared to unassisted healing
- Maintain better soft tissue contours
- Provide a more favorable ridge for delayed implant placement
The "almost always" qualifier: Ridge preservation makes sense when:
- You're not placing an immediate implant
- The patient needs time for decision-making
- Systemic factors contraindicate immediate surgery
- The socket anatomy is unfavorable
When to skip ridge preservation:
- Immediate implant with simultaneous grafting planned
- Socket shield technique selected
- Financial constraints (though this is unfortunate)
Clinical takeaway: Default to ridge preservation after extractions unless you have a specific reason not to. The cost is modest; the benefit to future implant placement is substantial. For a comprehensive, evidence-based approach to this procedure, see our complete guide on socket preservation techniques and alveolar ridge preservation.
Fact 6: Connective Tissue Grafts in Immediate Implants Enhance Outcomes
The science: If bone changes are inevitable, what about soft tissue? Here's where we CAN make a significant difference.
Connective tissue grafts (CTG) placed simultaneously with immediate implants provide:
- Increased soft tissue volume — Compensates for the buccal contour loss from bone resorption
- Enhanced keratinization — Creates more robust peri-implant tissue
- Improved tissue thickness — Better concealment of underlying implant/abutment
Multiple studies show that CTG combined with immediate implants produces superior aesthetic outcomes compared to immediate implants alone.
The technique matters: The CTG should be positioned to:
- Cover the buccal gap
- Extend beyond the implant shoulder
- Integrate with the existing keratinized tissue
Clinical takeaway: In the aesthetic zone, consider CTG as standard protocol for immediate implants, not an optional add-on. The soft tissue is often the difference between an acceptable result and an excellent one.
Fact 7: Socket Shield Technique Preserves What Matters
The science: If bundle bone is tooth-dependent, what if we kept part of the tooth? This is the elegant logic behind the socket shield technique.
By retaining the buccal root fragment (and its attached periodontal ligament), we maintain:
- Blood supply to the bundle bone
- Sharpey's fiber insertions
- The biological apparatus that keeps bundle bone alive
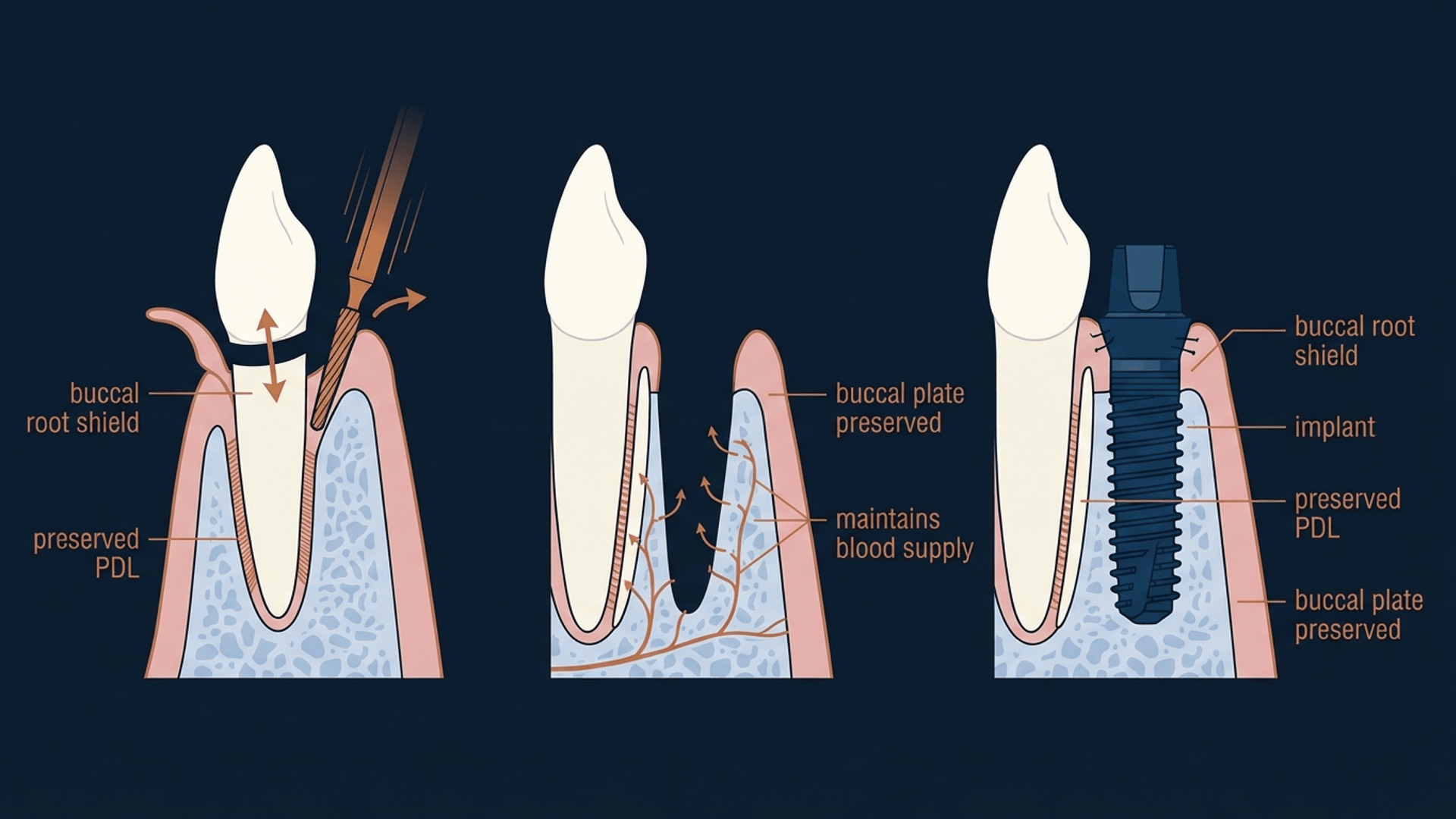
[Image generated with Periospot Studio]
First described by Hürzeler et al. (2010), the socket shield has evolved from experimental to mainstream, with growing evidence supporting its effectiveness.
What the research shows:
- Significantly better buccal bone preservation
- Reduced soft tissue recession
- Maintained papilla height
- High implant survival rates (comparable to conventional protocols)
The controversy: Socket shield isn't universally accepted. Critics point to:
- Technique sensitivity
- Risk of shield mobility or infection
- Limited long-term data (though this is improving)
Clinical takeaway: Socket shield represents a paradigm shift in how we think about extraction and implant placement. It's not for every case, but when indicated, it may be the closest we can get to true bundle bone preservation.
Fact 8: The Gap — 2mm Is Your Magic Number
The science: The "gap" refers to the space between the implant surface and the buccal socket wall. This gap is created intentionally by placing the implant in a palatal/lingual position.
The 2mm rule: Research suggests that a horizontal gap of approximately 2mm between the implant and the buccal plate is optimal. This allows:
- Space for bone regeneration or grafting
- Blood clot formation and stabilization
- Protection of the thin buccal plate from direct implant contact
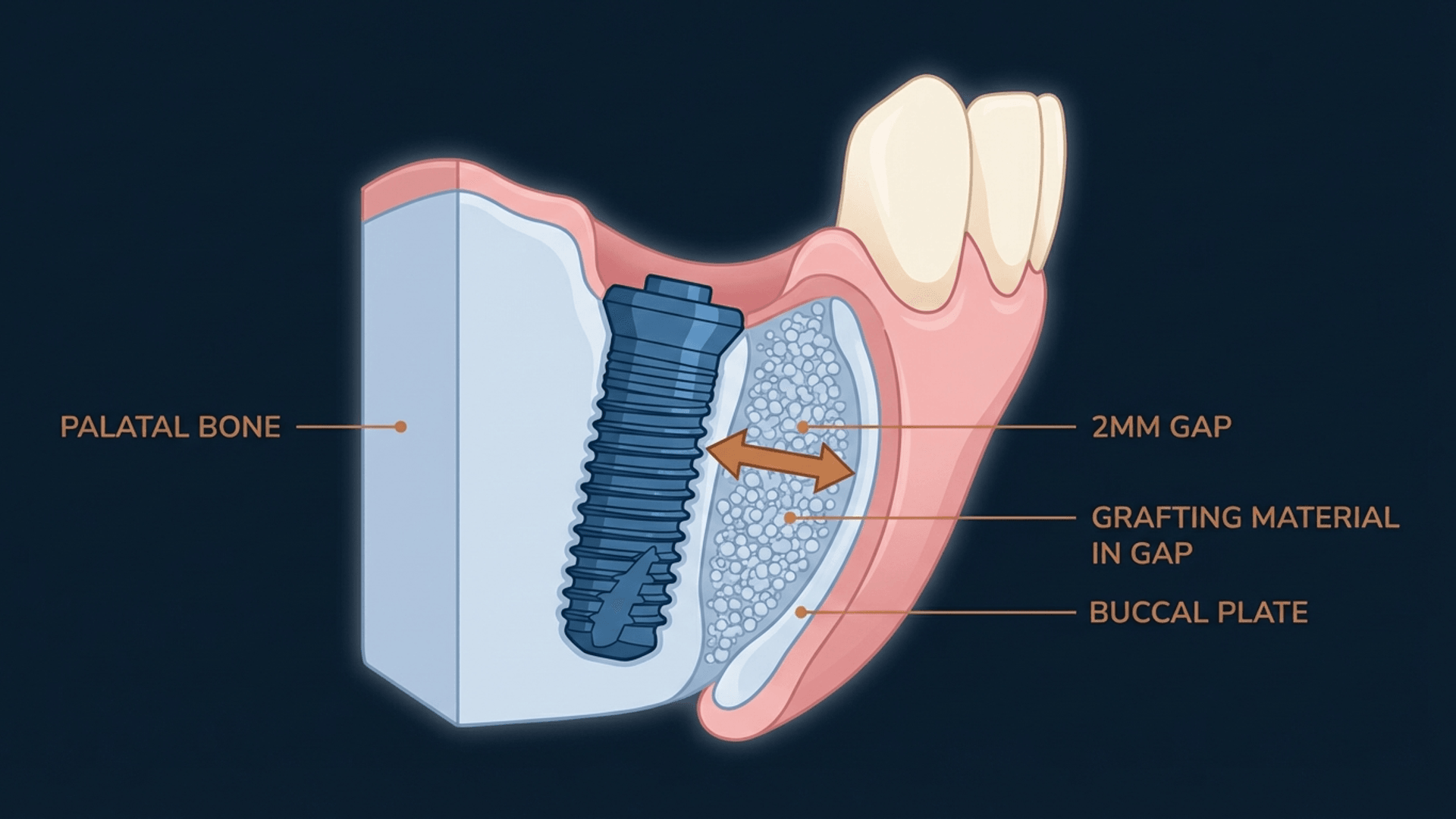
[Image generated with Periospot Studio]
Why position matters: If you place the implant too close to the buccal plate:
- Direct pressure accelerates resorption
- No space for grafting material
- Higher risk of thread exposure
If the gap is too large (>3mm):
- May require more extensive grafting
- Longer healing time
- Risk of incomplete bone fill
Clinical takeaway: When planning immediate implants, aim for 2mm buccal gap. This means the implant diameter selection and 3D positioning are critical. Use CBCT planning—don't estimate.
Fact 9: Implant Position — Where Biology Meets Restoration
The science: The "ideal" implant position balances:
- Biological requirements — Adequate bone support, healthy soft tissue
- Restorative requirements — Screw access, emergence profile, aesthetics
In immediate implants, this balance is even more critical because you're working within the constraints of an existing socket.
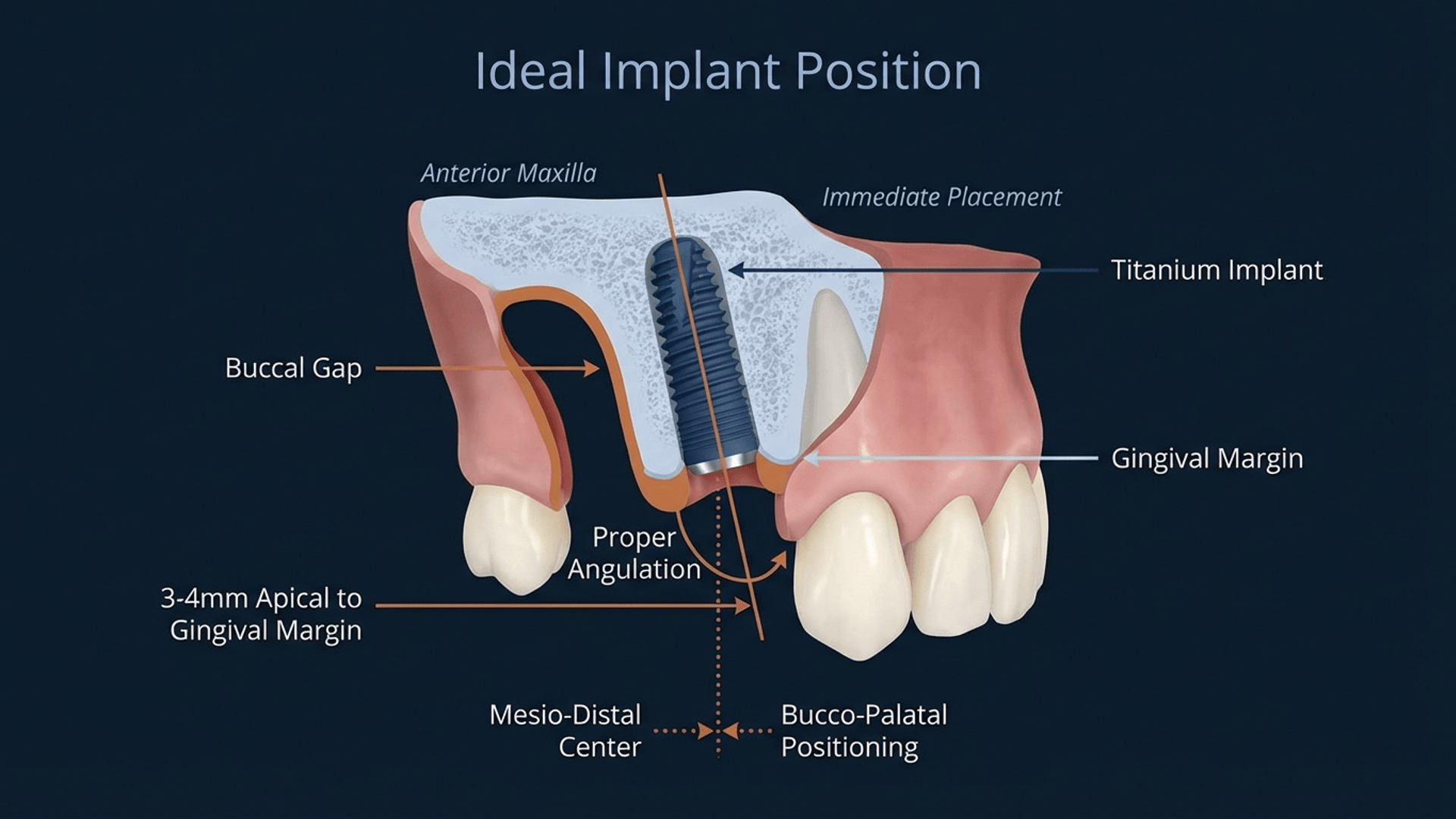
[Image generated with Periospot Studio]
The optimal position for anterior immediate implants:
- Mesio-distal: Centered in the socket, respecting adjacent root proximity
- Bucco-palatal: Palatal to the extraction socket axis (creating the 2mm buccal gap)
- Apico-coronal: 3-4mm apical to the planned gingival margin
- Angulation: Following the natural tooth axis or slightly palatally inclined
The emergence profile consideration: Your implant position determines your emergence angle. A palatal position allows for a more natural emergence from under the soft tissue, mimicking the cervical anatomy of a natural tooth.
Clinical takeaway: Don't chase primary stability at the expense of proper positioning. It's better to stage the procedure than to place an implant in a compromised position.
Fact 10: Narrow Implants — Sometimes Less Is More
The science: The average maxillary lateral incisor is approximately 7.21mm in mesio-distal width at the CEJ. Yet many clinicians reach for standard 4.3mm or even 5mm diameter implants.
The math doesn't work: A 4.3mm implant in a 7.21mm space leaves minimal room for proper emergence profile development. The restoration looks "too round" at the gingival margin.
When to go narrow:
- Lateral incisors
- Lower incisors
- Congenitally small teeth
- Limited interdental space
- Thin biotypes
Modern narrow implants (3.0-3.5mm) offer:
- Adequate strength for anterior applications
- Better emergence profile possibilities
- Less bone removal during osteotomy
- More conservative approach overall
Clinical takeaway: Match implant diameter to tooth anatomy, not to your inventory. Narrow implants in narrow spaces produce better aesthetic results.
Fact 11: Filling the Gap — The 0.4mm Threshold
The science: Here's a fascinating biological finding: gaps smaller than 0.4mm can heal spontaneously without grafting material.
This phenomenon relates to the critical size defect concept—below a certain dimension, the body can bridge the gap with new bone without external scaffolding.
Clinical implications:
- Very small gaps (jumping distance less than 0.4mm) may not require grafting
- Larger gaps benefit from biomaterial scaffolding
- The 2mm buccal gap definitely requires graft material
What to use for grafting:
- Xenografts (Bio-Oss, etc.): Most documented, slow resorption
- Allografts: Good integration, variable resorption
- Autogenous bone: Gold standard biology, limited availability
- Combinations: Often provide optimal results
Clinical takeaway: Don't over-complicate small gaps, but don't ignore the 2mm buccal gap either. Graft it. Every time.
Fact 12: The Paradigm Shift — Contact Inhibition Changes Everything
The science: This final fact represents the cutting edge of our understanding. The concept of contact inhibition in bone healing has significant implications for implant placement.
With contact inhibition: When an implant surface directly contacts bone, the healing pattern follows the implant surface. Bone cells "see" the implant and organize around it.
Without contact inhibition: When a gap exists, bone healing proceeds from the socket walls independently, then integrates with the implant surface.
Why this matters: Understanding this mechanism helps explain:
- Why primary stability isn't the only factor in success
- How gap healing actually works
- Why certain surface treatments and implant designs perform differently
The paradigm shift: We've moved from "implant must touch bone everywhere" to "strategic gaps with appropriate management yield better outcomes."
Clinical takeaway: Embrace the gap. Manage it properly with grafting and time, and you'll achieve better long-term results than forcing the implant against a thin buccal plate.
Clinical Decision Framework: Putting It All Together
Now that you understand the 12 facts, how do you apply them clinically? Here's my decision framework:
Assessment Phase
- CBCT analysis — Measure buccal bone thickness
- Soft tissue evaluation — Biotype, keratinized tissue width
- Patient factors — Expectations, healing capacity, compliance
Decision Points
Buccal bone greater than 1mm with favorable anatomy → Immediate implant candidate
- Plan for 2mm buccal gap
- Prepare for buccal grafting
- Consider CTG for aesthetic zone
Buccal bone less than 1mm with thin biotype → Staged approach recommended
- Ridge preservation at extraction
- Allow 3-4 months healing
- Delayed implant with potential GBR
Socket shield candidate criteria:
- Intact buccal root
- No periapical pathology
- Restorable emergence profile
- Experienced surgeon
Frequently Asked Questions
What is bundle bone in dentistry?
Bundle bone is the thin layer of alveolar bone proper that lines the tooth socket, characterized by Sharpey's fiber insertions from the periodontal ligament. It is tooth-dependent tissue that cannot survive without the presence of a tooth root.
Why does bundle bone resorb after tooth extraction?
Bundle bone receives approximately 70% of its blood supply from the periodontal ligament. When a tooth is extracted, this blood supply is severed, triggering inevitable osteoclastic resorption of the bundle bone.
What is the gap in immediate implant placement?
The gap refers to the horizontal space between the implant surface and the buccal socket wall. A gap of approximately 2mm is recommended to allow space for grafting and to protect the thin buccal plate from pressure-induced resorption.
Do immediate implants preserve bone?
No. Research clearly demonstrates that immediate implant placement does not prevent bundle bone resorption. Implants are prosthetic anchors, not bone-preserving devices. However, immediate implants offer advantages in treatment time and soft tissue maintenance.
Should you graft the gap in immediate implants?
Yes, for gaps larger than 0.4mm. The 2mm buccal gap recommended in immediate implant protocols should always be grafted with an appropriate biomaterial to provide scaffolding for bone regeneration.
What is the socket shield technique?
Socket shield involves retaining the buccal portion of the root with attached periodontal ligament during extraction and implant placement. This maintains blood supply to the bundle bone, potentially preserving the buccal plate better than conventional immediate implant protocols.
How much bone is lost after tooth extraction?
Studies show approximately 50% horizontal bucco-lingual reduction and 2-4mm vertical reduction within the first 12 months after extraction, with the majority occurring in the first 3 months.
Can bundle bone be preserved?
Complete preservation is not possible once a tooth is extracted. However, socket shield technique can maintain the bundle bone by retaining part of the tooth root. Ridge preservation procedures can minimize but not eliminate dimensional changes.
Key Takeaways
Understanding bundle bone biology transforms how you approach immediate implant cases:
- Bundle bone is tooth-dependent — Accept this biological reality
- Expect 50% buccal width reduction — Plan for it, don't be surprised by it
- Immediate implants don't preserve bone — They offer other advantages
- The 2mm gap is intentional — Position implants palatally
- Always graft the buccal gap — No exceptions in aesthetic cases
- CTG enhances outcomes — Consider it standard protocol anteriorly
- Socket shield is a valid option — When properly indicated
- Match implant diameter to anatomy — Narrow implants for narrow teeth
- Ridge preservation when not placing immediately — Default position
- Understanding biology improves decisions — These 12 facts guide every case
Conclusion
Twenty years after Chen, Araújo, and Lindhe published their foundational research, we understand bundle bone biology better than ever. The evidence is clear: bundle bone is tooth-dependent, extraction triggers inevitable resorption, and immediate implants are management tools, not preservation miracles.
But here's the good news: armed with this knowledge, you can achieve predictable, aesthetic outcomes.
The 12 facts in this guide aren't limitations—they're guideposts. They tell you what to expect, when to intervene, and how to manage the biology rather than fight against it.
Master the bundle bone, respect the gap, and embrace evidence-based protocols. Your patients—and their smiles—will thank you.
References
Araújo, M. G., and Lindhe, J. (2005). Dimensional ridge alterations following tooth extraction. An experimental study in the dog. Journal of Clinical Periodontology, 32(2), 212-218.
Chen, S. T., Wilson Jr, T. G., and Hämmerle, C. H. (2004). Immediate or early placement of implants following tooth extraction: review of biologic basis, clinical procedures, and outcomes. International Journal of Oral and Maxillofacial Implants, 19(Suppl), 12-25.
Hürzeler, M. B., et al. (2010). The socket-shield technique: a proof-of-principle report. Journal of Clinical Periodontology, 37(9), 855-862.
Araújo, M. G., Sukekava, F., Wennström, J. L., and Lindhe, J. (2006). Tissue modeling following implant placement in fresh extraction sockets. Clinical Oral Implants Research, 17(6), 615-624.
Tarnow, D. P., Chu, S. J., Salama, M. A., et al. (2014). Flapless postextraction socket implant placement in the esthetic zone. International Journal of Periodontics and Restorative Dentistry, 34(6), 781-787.
Schwarz, F.,3 By Giongo, M., and By Bot, J. (2022). Impact of the socket-shield technique on hard and soft tissue healing. Clinical Oral Implants Research, 33(5), 467-477.
Comments
0 totalLoading comments...
Previous
Bone Remodeling After Tooth Extraction: Understanding the Healing Process in Implant Dentistry
Next
Test Post from Claude Desktop
Related Articles

Machine Learning for Dentists: Predicting Implant Success with AI
1 min read
Osseointegration: The Stuff That Actually Makes Dental Implants Work (And Why You Should Care)
13 min read
